2816
3D MR black-blood thrombus imaging for the diagnosis of acute deep vein thrombosis at 1.5 T: a feasibility study1Shenzhen Institutes of Advanced Technology, Chinese Academy of Sciences, Shenzhen, People's Republic of China, 2Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 3Department of Radiology, Guangzhou Panyu Central Hospital
Synopsis
Accurate diagnosis of acute deep vein thrombosis (DVT) is relevant for appropriate treatment and avoiding life-threatening events. Recently proposed MR black-blood thrombus imaging (BTI) has demonstrated the potential to provide high sensitive and specific diagnosis of DVT. However, previous studies were performed at 3T and patients investigated were all in subacute to chronic phases. It remains unclear that if BTI could be used for the diagnosis of acute DVT and could work at 1.5T. Therefore, we sought to prospectively assess whether BTI is feasible at 1.5T for diagnosis of acute DVT, using contrast-enhanced MR venography as the standard reference.
PURPOSE
Accurate diagnosis of acute deep vein thrombosis (DVT) is relevant for prescribing prompt and appropriate treatment and avoiding life-threatening events1. Because of non-specific clinical symptoms of DVT, diagnosis of DVT relies on objective tests such as ultrasonography and contrast-enhanced CT or MR venography (CE-MRV)2. Recently, an MR black-blood thrombus imaging (BTI) technique was developed for the diagnosis of DVT3. The technique combines a black-blood preparation, i.e delay alternating with nutation for tailored excitation (DANTE), and a 3D variable-flip-angle turbo-spin-echo readout to achieve robust signal suppression of venous blood flow. As a result, thrombus can be directly visualized within the dark venous lumen without the need for contrast medium. Previous studies have demonstrated the potential of BTI for high sensitive and specific diagnosis of DVT3,4. However, results were available at 3T only and patients previously investigated were all in subacute to chronic phases. Thrombus in the acute phase may have rather long T1 but short T2 relaxation time due to the presence of intracellular methemoglobin5, and thus its signal intensity would be lower than that in the subacute or chronic phase. Furthermore, signal attenuation in static tissues by the DANTE preparation6 and overall lower signal-to-noise ratio at 1.5T versus 3T would also make the signal intensity of acute thrombus even lower. In this study, we sought to prospectively assess the feasibility of using BTI to diagnose acute DVT, with CE-MRV as the standard reference.METHODS
Experiments:
The IRB approved study consecutively enrolled 18 suspected acute patients (5F, 13M, age 57.9±15.6 y). The average duration from symptom onset to MR scan was 7.2±4.0 days (range, 2-14). The patients underwent three-station BTI to cover bilateral lower limbs. CE-MRV was also conducted to provide a standard reference. Imaging parameters of BTI and CE-MRV were shown in Table 1.
Image Analysis:
All images were loaded to a workstation (Avanto, Siemens,
Germany) for image analysis. Apparent signal-to-noise ratio (SNR) and contrast-to-noise
ratios (CNR) were calculated to demonstrate if BTI can provide adequate
thrombus signal for the diagnosis. Two readers blindly assessed the randomized
MR images and reported an independent diagnosis on the presence or absence of
thrombus on the per-segment level. Diagnostic confidence was scored (1: worst;
4: best) independently by the two readers for both BTI and CE-MRV. The
sensitivity (SE), specificity (SP), positive and negative predictive values
(PPV and NPV), and accuracy (ACC) of BTI were then calculated using the
consensus CE-MRV diagnosis as reference. Paired-sample t test was used for comparison among continuous variables.
Interobserver agreement and agreement between BTI and the consensus CE-MRV were
also tested using the Cohen κ test. p
< 0.05 indicated statistical significance.
RESULTS
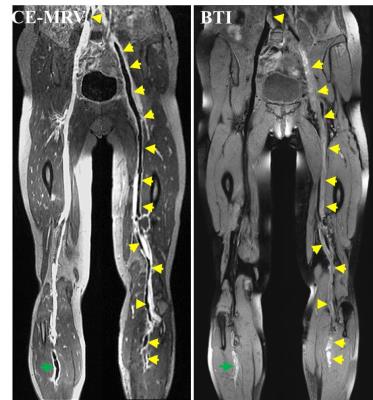
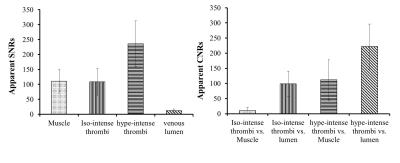
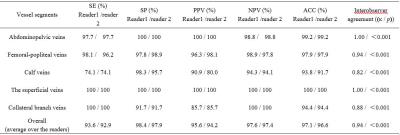
All participants successfully completed the MR scans. The thrombus in the acute phase appeared as iso- and/or hyper-intense signals on BTI images (Figure 1). The thrombus detected by BTI matched well with that by CE-MRV. According to the apparent SNR and CNR analysis, both iso- and hyper-intense thrombi exhibited adequate signal intensities and contrast for diagnosis (Figure 2). The diagnostic confidence of BTI was comparable with that of CE-MRV (average over the two readers: 3.71±0.61 vs. 3.73±0.55, p=0.44). High overall SE, SP, PPV, NPV and ACC as well as interobserver agreement were obtained (Table 2). Excellent agreement between BTI and CE-MRV was also achieved (reader1/reader2, κ = 0.94/0.92, p<0.001/p<0.001).DISCUSSION
BTI has capability to detect the acute DVT at 1.5T and may have a specific role in several scenarios for the diagnosis of DVT. First, BTI with three-station scan can cover the whole bilateral lower limbs, which is important for the diagnosis of asymptomatic DVT. In this study, DVT was detected in the asymptomatic contralateral legs of 2 patients which was missed in the initial ultrasonography examination. Second, the thrombus is frequently occurred in the pelvis for the pregnant DVT patients. However, current techniques, including US, CE-MRV and contrast venography, still have limitations in assessing the DVT in pelvis. These techniques used in pelvis have either low SE/SP or need contrast medium. In contrast, high SE (97.7%) and SP (100%) in abdominopelvic segments was achieved by the contrast-free BTI technique. Last but not least, the recurrence rate of DVT remains high (20%-40%). It is necessary to evaluate the progression of DVT with further complications such as pulmonary embolism. As a noninvasive, contrast-free and time-efficient technique, BTI could be a suitable tool for this.CONCLUSION
It is feasible to use BTI for the diagnosis of acute DVT at 1.5T. BTI has the potential to serve as a highly sensitive and specific contrast-free MR approach in DVT diagnostic work-up.Acknowledgements
This work was supported in part by American Heart Association (15SDG25710441), National Key Research and Development Program of China (2016YFC0100302), the National Science Foundation of China (81571669), the Natural Science Foundation of Shenzhen (JCYJ20160331185933583, GJHZ20150316143320494, KQCX2015033117354154), and the Natural Science Foundation of Guangdong (2014B030301013)References
1. Janssen MC, Wollersheim H, Schultze-Kool LJ, Thien T. Local and systemic thrombolytic therapy for acute deep venous thrombosis. Neth J Med. 2005;63(3):81-90
2. Huisman MV, Klok FA. Diagnostic management of acute deep vein thrombosis and pulmonary embolism. Journal of thrombosis and haemostasis : JTH. 2013;11(3):412-22
3. Chen H, Xie G, Liang J, et al. Diagnosis of deep vein thrombosis using 3D black-blood thrombus imaging (BTI): preliminary clinical experience. Journal of Cardiovascular Magnetic Resonance, 2016, 18(1): 1
4. Xie G, Chen H, He Z, et al. 3D black-blood thrombus imaging (BTI) for the diagnosis of deep vein thrombosis: initial clinical experience. Singapore, Proc. Intl. Soc. Mag. Reson. Med. 24 (2016): 0408
5. Bradley WG, Jr. MR appearance of hemorrhage in the brain. Radiology. 1993;189(1):15-26
6. Li L, Miller KL, Jezzard P. DANTE-prepared pulse trains: a novel approach to motion-sensitized and motion-suppressed quantitative magnetic resonance imaging. Magnetic resonance in medicine. 2012;68(5):1423-38
Figures