2806
Improved 3D phase contrast MR angiogram calculation using 3D CINE bSSFP and 4D flow MRIKelly Jarvis1,2, Susanne Schnell1, Alex J. Barker1, Shivraman Giri3, Nivedita Naresh1, James C. Carr1, Jeremy D. Collins1, and Michael Markl1,2
1Department of Radiology, Northwestern University, Chicago, IL, United States, 2Department of Biomedical Engineering, Northwestern University, Chicago, IL, United States, 3Siemens Healthcare, Chicago, IL, United States
Synopsis
Improvements in the 3D PC-MRA calculated from 4D flow MRI are needed for better vessel wall depiction and assessment of vascular dimensions. Balanced steady state free precession (bSSFP) is a promising imaging method to combine with 4D flow for an improved depiction of cardiac anatomy and blood-tissue contrast. This study of 10 healthy subjects compares multiple PC-MRA algorithms using bSSFP with 4D flow magnitude and flow images.
PURPOSE
For 4D flow MRI vessel boundaries can be depicted by a 3D phase contrast MR angiogram (PC-MRA), calculated from 4D flow magnitude and flow images. However, this approach is limited by the low blood-tissue contrast of 4D flow magnitude images. Balance steady state free precession (bSSFP) has inherently improved blood-tissue contrast for depicting cardiac anatomy1,2. We have developed a fast k-t accelerated 3D CINE bSSFP imaging protocol for use with 4D flow MRI. The purpose of this study was to use bSSFP with 4D flow MRI for an improved 3D PC-MRA calculation without significantly increasing scan time.METHODS
Non-contrast free-breathing k-t GRAPPA accelerated 3D CINE bSSFP MRI and 4D flow MRI were acquired using prototype sequences in 10 healthy subjects (aorta; age=44±18[21-68] years) at 1.5T (MAGNETOM Area, Siemens Healthcare, Erlangen, Germany) with the same spatial resolution (2.3-2.5 x 2.3-2.5 x 2.4 mm3) and volumetric coverage (FOV = 360-400 x 270-300 mm2, slab thickness = 72 mm) (Figure 1); the study was approved by institutional review board and all subjects gave informed consent. Three averages were acquired for 3D CINE bSSFP to mitigate breathing effects (outer mode averaging, TE = 1.6 ms, TR = 3.2 ms, temporal resolution = 38.4 ms, flip angle = 47-90 deg, R = 5, average scan time = 2.6 min) and interpolated along the temporal domain for integration with 4D flow (TE = 2.4-2.5 ms, TR = 4.8-4.9 ms, temporal resolution = 38.4-39.2 ms, flip angle = 7˚, GRAPPA acceleration with R = 2, venc=1.5 m/s). 3D PC-MRA was calculated using multiple algorithms with 4D flow and bSSFP data (Table 1). The standard deviation of the 4D flow velocity magnitude over time was used to suppress the high signal fat voxels in bSSFP. Contrast ratios were determined for ROIs in the aorta, septum, fat, liver and lungs. The algorithms that included bSSFP were compared to similar algorithms using 4D flow only (e.g. PC-MRA 3 was compared to 1 and 2).RESULTS
Scan times were average [range] = 4D flow: 11.2 [6.9-14.5], bSSFP: 2.6 [1.8-3.1] minutes. An example of images from one subject (Figure 2) and contrast ratios for all subjects (Figure 3) are shown. The contrast between the vessels and the septum, liver and lungs showed improvements when using bSSFP (PC-MRAs 3, 6, 9 and 12). The contrast between the aorta and the fat decreased when using bSSFP but could be improved using histogram equalization of the magnitude and bSSFP data prior to 3D PC-MRA calculation.DISCUSSION
These preliminary results indicate the potential for combining bSSFP and 4D flow MRI for improved 3D PC-MRA quality while adding only minimal scan time (2-3 minutes). Current limitations include incomplete removal of high intensity bSSFP fat signal and additional algorithms need to be explored for improved fat suppression in order to increase vessel-tissue and vessel-background contrast. In addition, the presented algorithms need to be studied in larger cohorts including patients with common aortic diseases.CONCLUSION
k-t GRAPPA accelerated 3D CINE bSSFP together with 4D flow MRI shows potential to improve the calculation of 3D PC-MRA. Future work will focus on the combination of these data for the best PC-MRA image quality for use in vessel segmentation.Acknowledgements
Grant support by NIH R01 HL115828 and K25 HL119608References
1. Scheffler K, Lehnhardt S. Eur Radiol. 2003;13(11):2409-2418.
2. Markl M, Leupold J. J Magn Reson Imaging. 2012;35(6):1274-1289.
Figures

Figure 1: One systolic slice of the 3D CINE bSSFP is shown with the corresponding slice in 4D flow MRI for magnitude and speed. The speed is the magnitude of the velocity vector. These time-resolved imaging volumes were combined into a 3D PC-MRA.

Figure
2: PC-MRA calculations 1-12 (a-l) are shown for one subject. On the left: time
averaged PC-MRA MIP, on the right: one slice of the PC-MRA. Algorithms using
bSSFP: 3, 6, 9, 12.
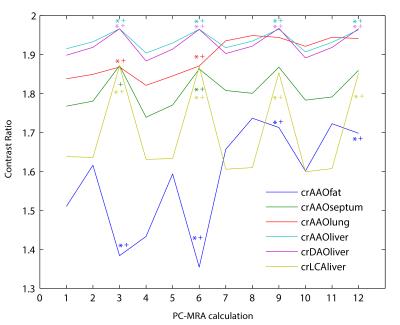
Figure 3: Contrast ratio
results as median in all subjects with the x-axis indicating the PC-MRA
algorithm used (12 algorithms from table 1). AAO: ascending aorta, DAO: descending
aorta, LCA: left common carotid artery (aortic branch). PC-MRAs with bSSFP (3,
6, 9, and 12) were compared to similar algorithms without bSSFP (1-2, 4-5, 7-8,
10-11, respectively). Symbols (* and +) indicate Wilcoxon signed rank paired test
p<0.05.
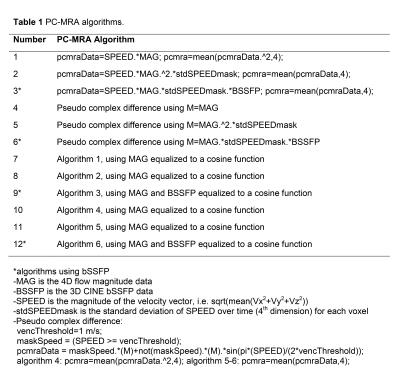
Table 1 PC-MRA algorithms