Robert R. Edelman1,2, Shivraman Giri3, Robert Silvers1, Kiran Thakrar1, and Ioannis Koktzoglou4,5
1Radiology, NorthShore University HealthSystem, Evanston, IL, United States, 2Radiology, Northwestern University, Chicago, IL, United States, 3Siemens HealthCare, 4Radiology, NorthShore University HealthSystem, 5Radiology, University of Chicago
Synopsis
For suspected
pulmonary embolism, CTA is the first-line imaging test, with CEMRA a potential
alternative. Disadvantages including
exposure to ionizing radiation and iodine contrast for CTA, while CEMRA is
sensitive to respiratory motion and requires a gadolinium-based contrast agent. As a nonenhanced alternative, we tested
breath-hold and free-breathing versions of single-shot radial QISS. Compared with the reference standard, all pulmonary
artery branches down to the segmental level were visualized by breath-hold and
navigator-gated QISS. With further optimization
and validation, radial QISS has the potential to provide a nonenhanced
alternative to CTA and CEMRA for the evaluation of suspected pulmonary
embolism.
Purpose:
For patients presenting to the emergency department
with chest pain, one of the most important considerations in the differential
diagnosis is pulmonary embolism.
Pulmonary embolism causes tens of thousands of deaths annually and has a
20% 90-day mortality rate. Unfortunately,
the symptoms are non-specific, so that imaging is often required to make an
accurate diagnosis. CT angiography has
replaced the radionuclide ventilation-perfusion scan as the mainstay of
diagnosis (1). While CTA provides
accurate evaluation of the pulmonary arteries, it exposes patients to ionizing radiation
and requires iodine contrast administration, which is contraindicated in
patients with impaired renal function. Contrast-enhanced
MR angiography (CEMRA) of the pulmonary arteries is a potential alternative (2). While eliminating radiation exposure, it
requires the administration of a gadolinium-based contrast agent which is contraindicated
in patients with impaired renal function as well as in pregnant women. Moreover, CEMRA requires a lengthy
breath-hold, which may not be feasible if the patient is dyspneic as is common
in pulmonary disorders such as pulmonary embolism. We therefore explored the feasibility of applying
nonenhanced MRA techniques to depict pulmonary arterial anatomy, using breath-hold
and free-breathing implementations of single-shot radial quiescent-interval
slice-selective (QISS) MRA (3).Methods:
This IRB-approved study was
conducted on a 1.5 Tesla scanner (MAGNETOM Avanto, Siemens Healthcare,
Erlangen, Germany). A prototype single-shot
radial QISS sequence was used for breath-hold and free-breathing acquisitions. Typical imaging parameters included: 97-99
radial views, field of view 260 mm, 3.1-mm slice thickness with 20% slice
overlap, 50-60 slices, 3 concatenations for breath-hold acquisitions. Free-breathing acquisitions used navigator
gating with a 3-mm navigator window and both leading and trailing navigators. In most subjects, both coronal and axial QISS
scans were acquired. Eight subjects were
studied including three healthy volunteers and five patients. For the volunteers, the reference standard
was CEMRA. In each of the volunteers, at
least one Cartesian QISS scan was acquired in addition to radial QISS in order
to evaluate the impact of k-space trajectory on image quality. The patients underwent CTA (which served as
the reference standard) on the same day as the MR exam in preparation for a pulmonary
vein isolation procedure to treat persistent atrial fibrillation. All patients had atrial fibrillation at the
time of the MRA study, with RR intervals ranging from ~500 ms to ~1200 ms. Source images and thin multi-planar
reconstructions were evaluated by two radiologists, each with more than five
years’ experience in the interpretation of pulmonary CTA and body MRA. Twenty-five pulmonary arterial segments were
scored for image quality in each subject.Results:
Typical breath-hold times were
~15-20 seconds. Scan times for
navigator-gated studies were ~2-3 minutes.
Comparing Cartesian and radial QISS MRA, the radial scans consistently
showed more uniform intravascular signal intensity and sharper vessel
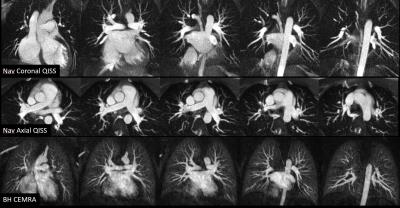
borders. Both breath-hold and
navigator-gated single-shot radial QISS MRA provided fair-to-excellent
evaluation of pulmonary arterial anatomy (Figure
1). All pulmonary arterial branches
down to the segmental level were visualized by breath-hold and navigator-gated
QISS. On an individual segmental basis,
no significant differences in image quality were found between the breath-hold
QISS, navigator-gated QISS and CEMRA protocols by either radiologist reader.
Aggregating data across all pulmonary arterial segments, both readers preferred
breath-hold QISS to navigator-gated QISS (P<0.05). Reader 1 preferred CEMRA
to both breath-hold and navigator-gated QISS (P<0.001), whereas reader 2
preferred breath-hold QISS to CEMRA (P<0.001). Inter-reader agreement was fair (kappa = 0.3)
for breath-hold QISS, and moderate (kappa = 0.46) for navigator-gated QISS and
CEMRA (kappa = 0.42). In patients using
CTA as the reference standard, breath-hold and navigator-gated QISS MRA
maintained diagnostic quality despite the irregular cardiac rhythm.Discussion and Conclusion:
In
this preliminary study, we found that both breath-hold and free-breathing
single-shot radial QISS MRA efficiently demonstrated pulmonary arterial anatomy
from the main pulmonary trunk through the level of the segmental branches. Navigator-gated acquisitions tended to show
mild blurring compared with breath-hold scans, but maintained diagnostic image
quality. The single-shot QISS technique
was also noted to be resistant to cardiac arrhythmias that were present in all
patients. Further studies will be
directed towards technique optimization, as well as to evaluating the
accuracy of the radial QISS technique in patients with suspected pulmonary
embolism. Acknowledgements
No acknowledgement found.References
1. Stein
PD, et al. N Engl J Med. 2006 Jun
1;354(22):2317. 2. Nagle SK, et al. Eur
J Radiol. 2016 Mar;85(3):553. 3. Edelman RR, et al. J Cardiovasc Magn Reson 2015 Nov 23;17:101.