2769
Predicting Procedure Successful Rate after Endovascular Recanalization for Chronic Carotid Artery Occlusion by 3D Vessel Wall Imaging1Radiology, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People's Republic of China, 2Neurosurgery, Renji Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People's Republic of China, 3MR Clinical Science, Philips Healthcare, Greater China, People's Republic of China, 4Center for Biomedical Imaging Research,Department of Biomedical Engineering, Tsinghua University, Beijing, People's Republic of China, 5University of Washington, WA, United States
Synopsis
Endovascular recanalization in patients with carotid chronic total occlusion (CTO) has been reported to be technically challenging. In this study, we retrospectively analyzed the 3D vessel wall imaging in patients with carotid CTO and its relationship to technical success rates. A total of 15 consecutive carotid CTO recanalization attempts were performed with overall technical success rate 60.0%. Compared with failure group, patients with an occlusion length <50mm, distal true lumen visibility in C1 segment on MR vessel wall images had a higher rate of successful recanalization. 3D vessel wall MR imaging may play a role in patient selection of endovascular recanalization in patients with carotid CTOs.
Introduction
The patient selection criteria for the treatment of carotid chronic total occlusion (CTO) are still controversial[1,2]. It is rare to find report about how to predict the technical success rates after endovascular recanalization using non-invasive technique such as MR imaging. In this study, we retrospectively analyzed the pre-procedural 3D vessel wall imaging in patients with carotid CTO and its relationship to technical success rates.Methods
Study sample: Patients who were diagnosed and confirmed with internal carotid artery CTOs by ultrasound or computed tomography, or conventional angiography were included in the study. MR imaging:3D vessel wall images were acquired using a whole body clinical scanner (Philips Achieva TX, the Netherlands) and a dedicated 8-channel phased-array carotid coil. 3D vessel wall sequences were acquired with the following parameters: (1)3D MERGE: the improved motion-sensitized driven-equilibrium (iMSDE) [3] prepared rapid gradient echo sequence, TR/ TE 9.3/4.4 ms, flip angle 6°, FOV 250[FH] ×160[RL]×64[AP] mm3, acquisition matrix 312×200×80, acquired resolution 0.8×0.8×0.8mm3, Rec resolution 0.4×0.4×0.4mm3, acquisition time 2 minutes 42 seconds; (2) 3D magnetization-prepared rapid acquisition gradient-echo (MP-RAGE) sequence, IR TFE, TR/TE 9.2/5.5 ms, flip angle 15°, acquisition time 1 minutes 55 seconds. Endovascular recanalization: The patients subsequently underwent endovascular recanalization within 1 week of the 3D vessel wall MR imaging. The endovascular recanalization procedure was performed, as previously described[4]. Patients were divided into two groups according to technical success or not of the endovascular recanalization. Data analysis: An experienced radiologist reviewed the carotid vessel wall images, and morphologic characteristics regarding the stump, occlusion length, intraplaque hemorrhage(IPH) over occluded segment and distal true lumen visibility in C1 segment were recorded.Results
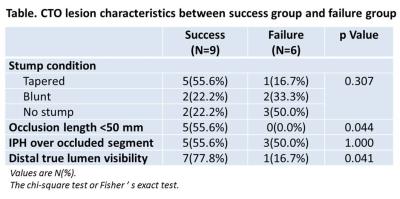
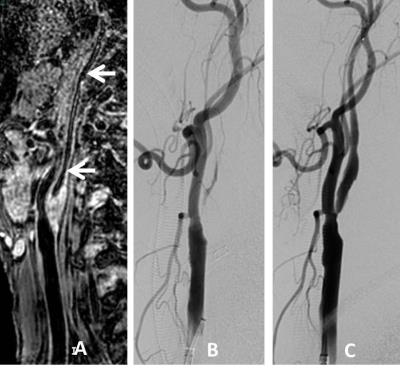
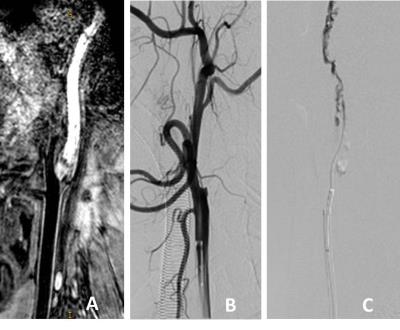
A total of 15 consecutive CAO recanalization attempts were performed in 14 patients (11 men; age 66.1 ±7.9 years). The one patient with bilateral occlusions was treated in two sessions. Nine arteries (9/15, 60.0%) were successfully recanalized. IPH was present in 53.4% (8/15) of the occlusions. An occlusion length of ≥50 mm was seen in 66.7% (10/15). Compared with failure group, patients with an occlusion length <50 mm, distal true lumen visibility in C1 segment had a higher rate of successful recanalization(Table, Fig.1,2).Discussion and conclusions
In this small sample size study, we analyzed the anatomic differences between the technical success and failure groups with internal carotid CTO. The results of our study suggest that patients with internal carotid CTOs that are with occlusion length <50 mm or distal true lumen visibility of the C1 segment on 3D vessel wall images are more appropriate candidates for recanalization. Our study had several limitations including its retrospective nature, and other factors (such as the length of time the vessel was occluded or the hemodynamic status) were not evaluated. Our findings indicate that 3D vessel wall MR imaging may play a role in patient selection of endovascular recanalization in patients with carotid CTOs, and this potential benefit should be proven to outweigh the risk of procedural complication in further investigations.Acknowledgements
None.References
1. Grubb RL Jr., Powers WJ, Clarke WR, et al. Surgical results of the carotid occlusion surgery study. J Neurosurg 2013;118:25-33.
2. M. Shojima, S. Nemoto, A. Morita, et al. Protected endovascular revascularization of subacute and chronic total occlusion of the internal carotid artery, AJNR Am. J. Neuroradiol. 2010;31(3): 481–486.
3. Wang J, Yarnykh VL, Yuan C. Enhanced image quality in black-blood MRI using the improved motion-sensitized driven-equilibrium (iMSDE) sequence. J Magn Reson Imaging. 2010;31(5):1256-63.
4. Zhao H, Wang J, Liu X, et al. Assessment of carotid artery atherosclerotic disease by using three-dimensional fast black-blood MR imaging: comparison with DSA. Radiology. 2015;274(2):508-516.
Figures