2757
An alternative T1 estimation algorithm with a higher flip angle improves T1 mapping accuracy and precision of the MOLLI sequence1Radiology, University of California, Los Angeles, Los Angeles, CA, United States, 2Division of Cardiology, University of California, Los Angeles, Los Angeles, CA, United States
Synopsis
Good T1 estimation accuracy and precision is important for clinical application of the myocardial T1 mapping technique. Although the widely used T1 mapping technique, modified Look-Locker
Background
Myocardial T1 mapping is an emerging technique used to assess diffuse myocardial fibrosis. Currently, the modified Look-Locker inversion-recovery (MOLLI) sequence (1) is widely used for myocardial T1 mapping due to its good precision and reproducibility (2,3). MOLLI uses a 3-parameter exponential fit with Lock-Locker correction for T1 estimation, which is known to underestimate T1 values and is sensitive to different parameters such as flip angle (FA) (4). Because higher flip angles will result in greater T1 underestimation, a lower FA=35° is commonly used to strike a balance between accuracy and precision (5). Several novel T1 estimation algorithms have been proposed to improve the T1 estimation accuracy of the MOLLI sequence (6–8). However, these algorithms have reduced T1 estimation precision. We sought to develop an improved myocardial T1 mapping technique that achieves better accuracy and precision than the standard MOLLI sequence by using a higher flip angle MOLLI with Bloch equation simulation and slice profile correction (BLESSPC) for T1 estimation.Methods:
The MOLLI pulse sequence was implemented on a 1.5T MRI scanner (Avanto Fit Siemens Healthcare; Erlangen, Germany). The 50° flip angle MOLLI with BLESSPC fit was compared to the 35° flip angle MOLLI with the original fit. The original fit refers to the conventional MOLLI T1 estimation algorithm with inversion factor correction (9). Researchers have proposed to use BLESSPC T1 estimation for the FLASH-MOLLI sequence (10). In the current work, we extend the BLESSPC algorithm to calculate T1 values based on the bSSFP- MOLLI sequence to achieve higher SNR. The signal evolution of bSSFP readouts are simulated using the Bloch equation. By assuming a fixed T2 = 45 ms, the modified BLESSPC remains a suitable fit with three parameters M0, T1 and FA.
Nine gel phantoms were used. Reference T1 for each gel phantom was determined by a standard inversion-recovery spin echo technique. MOLLI sequences using FA=35° and 50° were performed at a simulated heart rate of 60 bpm. The two sequences were repeated five times to evaluate T1 estimation precision. In eight healthy volunteers, images of the mid-left ventricular (mid-LV) short-axis were acquired using the same MOLLI sequences at FA=35° and 50°, which were repeated once to evaluate the intra-scan reproducibility. For each MOLLI scan, two T1 maps were generated using the original fit and the BLESSPC fit. The same inversion factor δ = 0.96 (9) was used in both phantom and in vivo studies. While the main focus is to compare the 50° MOLLI with BLESSPC fit to the 35° MOLLI with the original fit. The other two T1 maps (FA=35° using BLESSPC fit and FA=50° using original fit) were generated to demonstrate that the BLESSPC fit is more robust than FA variations when compared to the original fit. In vivo reproducibility was calculated as the absolute difference in the ROI-averaged T1 divided by the average of the repeated scans.
Results
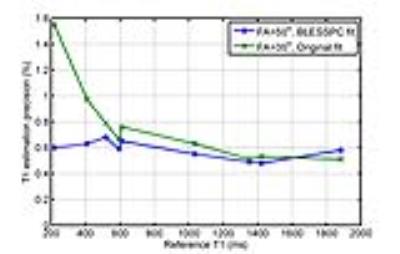
Figure 1 and 2 shows comparative phantom examples of T1 estimation accuracy and precision using the proposed technique (50° MOLLI with BLESSPC fit) vs. the standard MOLLI (35°, with the original fit). Compared to the standard MOLLI, the proposed technique provided better accuracy (0.5%±1.6% vs. -3.2%±1.4%) and precision (0.58%±0.07% vs. 0.77%±0.33%) for T1 values ranging from 218 ms - 1884 ms. Figure 1 also shows that the original fit produced larger T1 underestimation at higher flip angle while the BLESSPC fit with MOLLI generated similar T1 estimation errors at FA = 35° and 50°.
Based on native myocardial T1 values from the interventricular septal region of eight volunteers, the proposed technique generated significantly higher T1 values compared to standard MOLLI (1052±26 ms vs. 1005±21 ms, relative 4.7%±1.3%, p<0.001). Native myocardial T1 maps obtained in one healthy volunteer using the two techniques and their corresponding selected ROIs are shown in Figure 3. In this volunteer, the proposed technique generated higher native myocardial T1 values than the standard MOLLI (1040±24ms vs 1007±34 ms). The intra-scan reproducibility of the proposed technique trended to be better than the standard MOLLI technique (0.52%±0.36% vs. 0.96%±0.68%, p = 0.06). In all volunteers, the myocardial T1 value was lower using MOLLI at a higher flip angle and with the original fit (971±23 ms for FA=50°, p < 0.001), whereas the BLESSPC fit was insensitive to flip angle changes (1046±20 ms for FA=35°, p= 0.2).
Conclusion
T1 estimation using BLESSPC fit and a MOLLI acquisition at FA=50° is superior to MOLLI at a FA=35° with the original fit in regards to accuracy and precision. Further clinical studies in varying pathologic conditions are warranted to confirm our findings.Acknowledgements
N/AReferences
1. Messroghli DR, Greiser A, Fröhlich M, Dietz R, Schulz-Menger J. Optimization and validation of a fully-integrated pulse sequence for modified look-locker inversion-recovery (MOLLI) T1 mapping of the heart. J. Magn. Reson. Imaging 2007;26:1081–6.
2. Roujol S, Weingärtner S, Foppa M, Chow K, Kawaji K, Ngo LH, Kellman P, Manning WJ, Thompson RB, Nezafat R. Accuracy, precision, and reproducibility of four T1 mapping sequences: a head-to-head comparison of MOLLI, ShMOLLI, SASHA, and SAPPHIRE. Radiology 2014;272:683–9.
3. Raman FS, Kawel-Boehm N, Gai N, Freed M, Han J, Liu C-Y, Lima JAC, Bluemke DA, Liu S. Modified look-locker inversion recovery T1 mapping indices: assessment of accuracy and reproducibility between magnetic resonance scanners. J. Cardiovasc. Magn. Reson. 2013;15:64.
4. Gai ND, Stehning C, Nacif M, Bluemke DA. Modified Look-Locker T1 evaluation using Bloch simulations: human and phantom validation. Magn. Reson. Med. 2013;69:329–36.
5. Kellman P, Hansen MS. T1-mapping in the heart: accuracy and precision. J. Cardiovasc. Magn. Reson. 2014;16:2.
6. Shao J, Nguyen K-L, Natsuaki Y, Spottiswoode B, Hu P. Instantaneous signal loss simulation (InSiL): an improved algorithm for myocardial T1 mapping using the MOLLI sequence. J. Magn. Reson. Imaging 2015;41:721–9.
7. Xanthis CG, Bidhult S, Kantasis G, Heiberg E, Arheden H, Aletras AH. Parallel simulations for QUAntifying RElaxation magnetic resonance constants (SQUAREMR): an example towards accurate MOLLI T1 measurements. J. Cardiovasc. Magn. Reson. 2015;17:104.
8. Sussman MS, Yang IY, Fok K-H, Wintersperger BJ. Inversion group (IG) fitting: A new T1 mapping method for modified look-locker inversion recovery (MOLLI) that allows arbitrary inversion groupings and rest periods (including no rest period). Magn. Reson. Med. 2016; 75:2332-40.
9. Kellman P, Herzka DA, Hansen MS. Adiabatic inversion pulses for myocardial T1 mapping. Magn. Reson. Med. 2014;71:1428–34.
10. Shao J, Rapacchi S, Nguyen K-L, Hu P. Myocardial T1 mapping at 3.0 tesla using an inversion recovery spoiled gradient echo readout and bloch equation simulation with slice profile correction (BLESSPC) T1 estimation algorithm. J. Magn. Reson. Imaging 2016;43:414–25.
Figures