2754
Free-breathing native cardiac T1 and T2 mapping with flexible elastic image registration: Preliminary Clinical Result1Philips Healthcare, Singapore, Singapore, 2National Heart Centre Singapore, Singapore, Singapore, 3Philips Healthcare, Japan, 4Philips Research, Hamburg, Germany, 5National Heart Centre Singapore, Singapore, 6Vanderbilt University, United States
Synopsis
Current myocardial T1 and T2 mapping based on inversion-recovery and single-shot readout techniques require generally at least 7 to 10 seconds breath hold. Improper and difficulties of breath hold is one of the main sources of error and reduced reproducibility. To mitigate the dependence of mapping on breath holds and also to increase patient comfort, we report free-breathing T1 and T2 mapping using different acquisition schemes using flexible elastic image registration. We demonstrate the feasibility of this approach with motion correction for increased image quality and quantification accuracy.
Introduction
MOLLI (modified Look-Locker inversion recovery)-based T1 mapping and T2prep-based T2 mapping are robust and widely used methods for myocardial tissue characterization. However, current approaches in clinical use requires reliable breath hold. Any motions may lead to misalignment between individual source images and hence poor map quality and reduced reproducibility 1,2. To mitigate the dependence of myocardial parametric mapping on breath holds and increase scan efficiency, here we demonstrated T1 and T2 mapping with different acquisition schemes using a novel approach for motion compensation.Materials and Methods
All patients underwent cardiovascular magnetic resonance (CMR) on a 3T system (Philips Ingenia). The protocol was approved by the local ethnic review board, and informed consent was obtained from each participant. All maps were acquired in the basal and mid-cavity short-axis level. For native T1 mapping three different MOLLI schemes were applied: 5s(3s)3s, 4s(1s)3s(1s)2s, and 3b(3b)3b(3b)5b, where the former two were latest development as second-based schemes for “native” and “enhanced” T1 mapping 1,3, while the last one was the “original” heartbeat-based version 4. T2-prepared single-shot sequence with non-selective composite pulses and three TET2prep times (0 ms, 24 ms, and 55 ms) as previously described was used for T2 mapping 2. All scans were performed with ECG-gated balanced steady-state free precession (bSSFP) contrast for both breath-hold and free-breathing, the acquisition order of which was randomized among subjects. The typical imaging parameters were: field of view 340 × 340 mm2, matrix size 188 × 168 pixels, acquired pixel size 1.8 × 2.0 mm2, interpolated to 1.3 x 1.3 mm2, slice thickness 8 mm; repetition time TR / echo time TE 2.3 / 1.15 ms; flip angle 30° for T1 mapping and 40° for T2 mapping, T1 minimal inversion time 87.7 ms; SENSE parallel imaging factor 2.2. A modified non-rigid, non-parametric registration method consisting of elastic registration steps was applied to generate motion-corrected T1 and t2 maps 5,6. Image quality improvement was categorized as excellent, moderate to mild, no improvement, and deterioration. T1 and T2 values were reported from an interventricular septal region of interest (ROI) on the parametric map as mean ± standard deviation (SD). Analysis of variance (ANOVA) was performed to detect significant difference.Results and Discussion
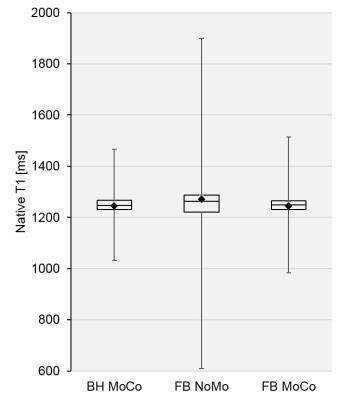
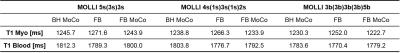
A total of 72 native T1 maps were obtained in 6 patients (mean age 43 ± 17 years, 5 males) with mixed cardiomyopathies for all three MOLLI schemes, while a total of 16 T2 maps were obtained in 4 healthy volunteers, for both breath-hold and free-breathing scans. In general, image quality in motion corrected free-breathing scans showed 24 cases (67%) excellent improvement and 12 cases (33%) moderate to mild improvement for T1 maps, while 16 (100%) moderate to mild improvement for T2 maps. Three examples were shown in Figures 1 and Figure 2, respectively. T1 values for the septal myocardium from all three schemes were summarized in Table 1. Both mean values as well as SD representing inter-subject variation (not shown here) did not show statistically significant difference (p>0.05) among all three schemes and among all three approaches, namely breath hold with motion correction as reference, free breathing without and with motion correction. However, intra-subject variations were dramatically reduced with proposed motion correction method for free-breathing T1 mapping for all three schemes, shown in Figure 3. In contrast to previous report 7, blood pool T1 values for the proposed method were not much different due to relative insensitivity of bSSFP contrast to inflow effect despite of 2D slice-selective readout. Left ventricular myocardium T2 values for breath-hold, free-breathing, and motion-corrected free-breathing scans were 41.0 ± 6.6, 47.2 ± 10.8, 43.1 ± 7.7 ms, respectively. While none of these three approaches showed significant difference to each other (p>0.05), respiratory-triggered acquisition may further improve accuracy in T2 mapping 2,8.Conclusion
We have demonstrated with preliminary clinical results the technical feasibility of myocardial T1 and T2 mapping during free breathing. The proposed method shows promise with warranted further validation in clinical studies.Acknowledgements
No acknowledgement found.References
1. Kellman P and Hansen M. J Cardiovasc Magn Reson 2014;16:2.
2. Giri S, et la. Magn Reson Med 2012;68:1570.
3. Higgins DM and Moon JC. Curr Cardiovasc Imaging Rep 2014;7:9252.
4. Messroghli DR, Radjenovic A, Kozerke S, et al. Magn Reson Med 2004;52:141-146.
5. Kabus S and Lorenz C. Proc MICCAI 13, 2010:81-89.
6. Le TT, Zhang S, Kabus S, et al. J Cardiovasc Magn Reson 2016; 18:176-178.
7. Jaime L. Shaw, Christodoulou AG, Sharif B, et al. Proc Intl Soc Mag Reson. Med 24, 2016; 3149.
8. van Heeswijk RB, et al. JACC Cardiovasc Imaging 2012;5:1231.
Figures