2747
Role of free-breathing motion-corrected phase-sensitive inversion recovery (MOCO-PSIR) imaging technique for the assessment of late gadolinium enhancement1Department of Radiology, Zhongshan Hospital, Fudan University, Department of Medical Imaging, Shanghai Medical school, Fudan University and Shanghai Institute of Medical Imaging, Shanghai, People's Republic of China, 2MR Research and Development, Siemens Healthcare, Los Angeles, CA, United States, 3Application development, Siemens Shenzhen Magnetic Resonance Ltd., Shenzhen, People's Republic of China
Synopsis
We aimed to investigate the role of motion-corrected phase-sensitive inversion recovery (MOCO-PSIR) technology for the evaluation of LGE. LGE imaging was conducted in 55 patients with MOCO-PSIR and conventional breath-hold PSIR sequences successively. Image quality was scored using a four-point scale. Compared with conventional PSIR, MOCO-PSIR showed better image quality and detected larger LGE volumes in nonischemic cardiomyopathy. Free-breathing motion-corrected PSIR method is a promising alternative to conventional PSIR sequence.
Purpose
To compare the image quality of a new free-breathing, motion-corrected phase-sensitive inversion recovery (MOCO-PSIR) technology with conventional breath-hold PSIR sequence, and to evaluate the MOCO-PSIR approach for the quantification of late gadolinium enhancement (LGE) volume using PSIR as reference standard.
Methods
Fifty-five patients with suspected cardiac diseases were enrolled. After administration of 0.2 mmol/kg Gd-DTPA, LGE imaging was conducted first with a prototype MOCO-PSIR sequence [1, 2], followed by a conventional breath-hold PSIR sequence using a 1.5T MR scanner (MAGNETOM Aera, Siemens, Erlangen, Germany). Same slice number(8 ~ 11 slices, varied among patients) of short-axis and three long-axis images were respectively obtained using these two methods. Image quality was graded by two independent reviewers using a four-point scale in which a score of 0 indicates poor, non-diagnostic, 1= fair, diagnostic may be impaired, 2= good, some artifacts but no impact on diagnostis, 3 = excellent, no artifacts. Scan time and LGE volume were compared between the two methods. Continuous data were compared by paired Student t test. The Wilcoxon signed-rank test was used to compare image quality between MOCO-PSIR and PSIR images. Interobserver agreement was expressed as the kappa score.Results
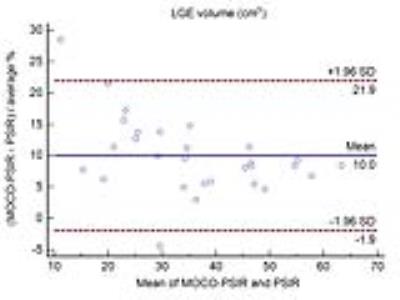
All images were interpretable. Scan time was significantly reduced from 301±35 seconds for PSIR to 176±27 seconds for MOCO-PSIR (P<0.001). Compared with conventional PSIR, the overall image quality of MOCO-PSIR was significantly improved [PSIR: 2 (interquartile range:1-2) vs. MOCO-PSIR: 3 (interquartile range: 2-3), P<0.001]. In patients with heart rate > 90bpm (n=12), image quality was also improved from 2(interquartile range: 1-2) to 3 (interquartile range: 2-3) (P<0.001) with MOCO-PSIR. The interobserver agreement of MOCO-PSIR was excellent with a kappa score of 0.88 (P<0.001), and there was a moderate interobserver agreement for the conventional PSIR technique (kappa score= 0.65, P<0.001). LGE was detected in 35 patients, including ischemic cardiac diseases in 6 cases and nonischemic cardiomyopathy in 29 cases. LGE volume was significantly larger in MOCO-PSIR compared with PSIR in patients suspected of nonischemic cardiomyopathy (37.3±13.9 cm3 vs. 34.1±13.3 cm3, P<0.001), whereas this was not true for ischemic cardiac disease (15.1±7.0 cm3 for MOCO-PSIR and 14.6±5.0 cm3 for PSIR, P=0.72). Furthermore, a Bland-Altman analysis confirmed a systematic larger LGE volume for the MOCO-PSIR method in nonischemic cardiomyopathy (10.0±11.9 %).Discussion
Our study indicated that the MOCO-PSIR imaging technique can significantly reduce scan time and improve image quality. Moreover, a larger LGE volume was measured using MOCO-PSIR compared with PSIR in patients with nonischemic cardiomyopathy. As we know, LGE lesions are frequently multifocal, diffuse, or faint in nonischemic cardiomyopathy [3]. We conjecture that the improvement in contrast-to-noise ratio in MOCO-PSIR leads to an improvement in quantification of LGE. LGE–MRI is a valuable technique for the evaluation of myocardial fibrosis in various cardiac diseases. However, the role of the conventional LGE technique is restricted in patients suffering from shortness of breath due to cardiac or pulmonary diseases. Therefore, a free-breathing sequence is especially useful in clinical practice.Conclusions
The free-breathing motion-corrected PSIR technique boasts better image quality and detects larger LGE volume in patients with nonischemic cardiomyopathy compared with a conventional PSIR sequence.Acknowledgements
No acknowledgement found.References
1. Piehler KM, etc., Cardiovascular Imaging 6, 423-4322. Flanagan O, etc., J Cardiovasc Magn Reson 16, P305
3. Kido T, etc., EUR J RADIOL 83, 2159-2166
Figures