2742
Assessment and detection of left ventricular thrombus in patients with acute ischemic stroke using cardiac MR (ADVENT study)1Department of Radiology, National Cerebral and Cardiovascular Center, Suita, Osaka, Japan, 2Division of Neurology, National Cerebral and Cardiovascular Center, Suita, Osaka, Japan, 3Division of Cardiology, National Cerebral and Cardiovascular Center, Suita, Osaka, Japan
Synopsis
In patients with acute ischemic stroke (AIS), the assessment of left ventricular thrombus (LVT) is essential. In this study, we showed the utility of the early phase of gadolinium enhancement for detecting LVT in AIS patients, which conventional TTE hardly identified. CE-CMR, when using the early phase of gadolinium enhancement, should be performed on acute ischemic stroke patients, especially those with prior myocardial infarction or LV dysfunction and without definitive stroke etiologies.
Introduction
Because patients with left ventricular thrombus (LVT) require anticoagulant therapy, the proper assessment of LVT is essential. Diagnostic workup for detecting cardioembolic sources of stroke commonly includes transthoracic echocardiography (TTE). However, TTE may not be enough to detect LVT. Contrast-enhancement cardiac magnetic resonance (CE-CMR) is useful for LVT detection among high-risk populations such as patients with myocardial infarction (MI) or left ventricular (LV) dysfunction. 1,2 However, CE-CMR is not widely used for detection of LVT in patients with acute ischemic stroke (AIS).Purpose
The aim of this study was to clarify the usefulness of contrast-enhanced cardiac MR (CE-CMR) in detecting left ventricular thrombus in patients with acute ischemic stroke.Methods
Among 448 consecutive AIS patients studied within 48 hours after onset, 50 patients both eligible for CE-CMR and at high risk of LVT (with prior myocardial infarction (MI) or LV dysfunction regarded as LVEF <50%) were prospectively enrolled. CE-CMR and conventional transthoracic echocardiography (TTE) were performed within 7 days of admission (5±2 vs. 3±2 days, respectively). CMR was performed using a 1.5 T scanner (Magnetom Sonata, Siemens, Erlangen, Germany). Contrast enhancement images for detection of LVT were acquired in the short- and long-axis slices encompassing the entire LV at 1–3 min after gadolinium administration (early phase of gadolinium enhancement). ECG gated 3D-IR-SSFP pulse sequence (True-FISP) was used with the following parameters: TR 3.5 ms, TE 1.7 ms, flip angle 60°, matrix 256×129, field of view 340 mm, slice thickness 3–5 mm, and inversion time 300 msec. The LV thrombus, which appeared as a low-signal intensity mass that was distinguishable from surrounding high-signal intensity structures, such as cavity blood and myocardial scarring, was independently diagnosed by two experienced observers who were blinded to the clinical history and other imaging tests. Cine images and late gadolinium enhancement (10–15 min after gadolinium injection) were also obtained for evaluation of cardiac function and the detection of myocardial damage (infarction or fibrosis) in a standardized clinical protocol. We compared the detection rate of LVT between CMR and TTE. Clinical characteristics and parameters of CE-CMR were also analyzed to predict LV thrombus.Results
This study enrolled 50 patients (42 men, 73±12 years old), including 27 (54%) patients with prior MI and 23 (46%) patients with LV dysfunction without ischemic heart disease. LV thrombi were identified in 9 (18%) by CE-CMR, whereas only 1 (2%) was detected by TTE (p = 0.031) (Table1). CE-CMR could identify smaller (< 1cm) thrombi located in either the apex or inferior wall, compared with TTE (Table 1). Patients with LVT showed significantly larger LV end-diastolic volume (p = 0.006) and lower LVEF (p < 0.001) than those without LVT (Table 2). LVT-positive patients had a higher prevalence of prior MI than LVT-negative patients (p = 0.047) (Table 2). After multivariate logistic regression analysis, cryptogenic stroke was independently associated with LVT (Table 3). Among 17 patients with an undetermined stroke etiology by routine examinations, 7 (41%) were determined to have apical thrombi via CE-CMR.Discussion
We showed the utility of CE-CMR for detecting LVT in AIS patients, which conventional TTE hardly identified. In the early phase of gadolinium enhancement, homogeneous and strong enhancement of the LV cavity allowed easy detection of LVT as an abnormal, dark structure adjacent to the enhanced myocardium. 3 CE-CMR was especially useful for detecting small apical thrombi in patients with prior MI and those without definitive stroke etiologies such as lacunar, atherosclerosis, and atrial fibrillation. Hence, CE-CMR is useful for diagnosing cardioembolic stroke and decision making regarding oral anticoagulants.Conclusion
CE-CMR was found to be a useful tool for detecting LVT in acute stroke patients when compared with conventional TTE. At-risk patients could be misdiagnosed with embolic strokes of unknown origin without CE-CMR. CE-CMR should be performed on both acute ischemic stroke patients with prior MI and those without definitive stroke etiologies.Acknowledgements
No acknowledgement found.References
1. Weinsaft JW et al. LV thrombus detection by routine echocardiography: Insights into performance characteristics using delayed enhancement CMR. JACC Cardiovasc Imaging. 2011 Jul;4(7):702-12.
2. Mollet NR et al. Visualization of ventricular thrombi with contrast-enhanced magnetic resonance imaging in patients with ischemic heart disease. Circulation. 2002 Dec 3;106(23):2873-6.
3. Delewi R et al. Left ventricular thrombus formation after acute myocardial infarction. Heart. 2012 Dec;98(23):1743-9.
Figures
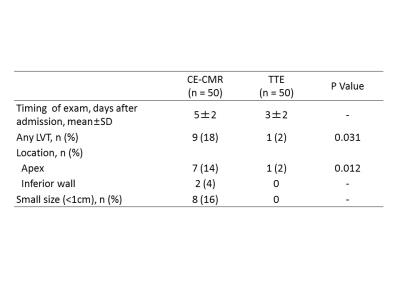
Figure 1. Representative cases of LVT assessed by CE-CMR and conventional TTE
A–C: CE-CMR. LVT (arrowhead) were detected in both the apex (A, B) and inferior wall (C);
a–c: conventional TTE. LVT (large apical thrombus, arrow) was detected in only one case (a).