2737
Prognostic value of cardiac MR imaging for end-stage phase of hypertrophic cardiomyopathy patients with or without adverse ventricular remodeling1Fuwai Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, People's Republic of China, 2Fuwai Hospital,Chinese Academy of Medical Sciences and Peking Union Medical College
Synopsis
Cardiac morphology as well as LGE extent proved to be particularly heterogeneous in ES phase of HCM patients. For ES phase of HCM patients with adverse ventricular remodeling, LGE was a significant predictor of poor outcomes. But for ES phase of HCM patients without ventricular dilatation, biatrial enlargement, extremely diastolic dysfunction and higher incidences of AF may contribute more to adverse prognosis.
Introduction
End-stage (ES) phase of hypertrophic cardiomyopathy (HCM) is a recognized part of the HCM disease spectrum. Previous literatures have described the clinical and CMR expressions. But the prognostic value of morphological parameters and precise extent of LGE derived from CMR remain unknown, especially in those cases without adverse ventricular remodeling. We quantitatively evaluated the CMR parameters and sought to explore the value of CMR for ES phase of HCM.Method
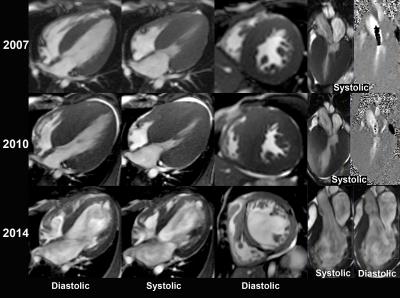
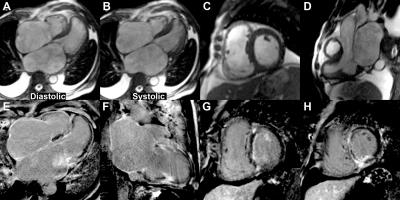
Of 2228 consecutive HCM patients, 63 were diagnosed as ES phase with systolic dysfunction (left ventricular eject function less than 50%). ES patients were divided into those with ventricular dilatation (D-ES, n=40) and those with normal ventricular size (N-ES, n=23). All of the patients were assessed by ultrasound and CMR. LGE were semi-automatic measured with the gray-scale threshold method at 5 SD above the mean signal intensity of normal myocardium. Regional LGE analyses were performed using 17-segments model. Cox proportional hazards models were used to assess the association between cardiac MR parameters and outcomes.Result
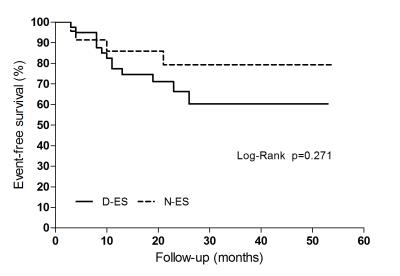
The left ventricular ejection function of D-ES (27.9±8.8)% were significantly lower than that of N-ES (35.0±7.5)% (p<0.05). AF was more common in N-ES than D-ES group (p<0.05). The volume fraction of LGE was significantly larger in patients with left ventricular dilatation (D-ES: 36.3%±14.6%; N-ES: 21.4%±8.7%) (p<0.05), especially in anterior and lateral wall. Over the follow-up period of 21.62±13.41 months, 17 patients experienced cardiovascular death/heart transplantation events (13 in D-ES, 4 in N-ES). Log-rank test found no significant difference between 2 groups in cardiovascular death/heart transplantation events (c2=1.211, p=0.271). There was a significant correlation between LGE volume fraction and cardiovascular death/heart transplantation in D-ES group (HR:1.62 per 10% LGE increase, p<0.05). But in N-ES group, left atrial diameter/left ventricular end-diastolic diameter (LAD/LVEDD) (HR 2.59 per 0.1 LAD/LVEDD increase, p<0.05) was an independent predictor of the outcomes.Discussion
Much of the previous literature about ES was confined to ventricle dilated phenotype. ES phase of HCM was considered to be characterized by impaired systolic function and increased volume of ventricles. But Harris et al. [1] reported that more than one third of the ES patients showed a nondilated or persistently hypertrophied LV or both. The results of this study showed that more than 1/3 patients manifested as normal ventricles, which was in line with previous study.
In addition, biatrial enlargement and higher incidences of AF were observed in the majority of patients without ventricle dilatation, which resembled to restrictive cardiomyopathy. Kubo et al. [2] identified a distinct part of HCM with “restrictive phenotype” characterized by restrictive filling, minimal or no hypertrophy, and preserved LV systolic function. Besides, restrictive filling proved to be a strong and independent predictor of subsequent evolution to the ES [3]. Although Kubo et al. didn’t find LV systolic dysfunction in all 6 patients before death; we cannot exclude the possibility that ES patients with normal ventricular dimension in this study were part of decompensation stage of HCM with “restrictive phenotype”.
Recent studies indicated that extent of LGE might be an effective tool for risk stratifying patients with HCM [4]. The present study also validated the predictive value of extent of LGE (HR 1.62 per 10% LGE increase, p<0.05) in ES phase of HCM patients with ventricular dilatation. It is worth noting that, compared with ES patients with ventricle dilatation, patients with normal ventricle size showed a relatively smaller amount of LGE, but there was no significant difference for endpoint events between two groups. For patients with adverse ventricle remodeling, the evolution is probably the consequence of progressive myocardial fibrosis [5,6] and microvascular dysfunction [7]. But for patients with normal ventricle size, the ratio of LAD/LVEDD (HR 2.59 per 0.1 LAD/LVEDD increase, p<0.05) was a significant predictor of endpoint events. We also found that ES patients with normal ventricle size showed much higher of AF prevalence (69.9%) than general HCM patients (22%) [8].Therefore, we believe that for patients with normal ventricle size, heart failure is possibly due to AF and severe diastolic dysfunction, which worsened the hemodynamics of a well-tolerated HCM.
Conclusion
Systolic dysfunction is a sine qua non of ES, whereas cardiac morphology as well as clinical expression of ES phase proved to be particularly heterogeneous in this study. For ES phase of HCM patients with adverse ventricular remodeling, LGE was a significant predictor of poor outcomes. But for those without ventricular dilatation, biatrial enlargement, extremely diastolic dysfunction and higher incidences of AF may contribute more to adverse prognosis. Despite the heterogeneous clinical and CMR characteristics, patients with ES phase of HCM may ultimately require heart transplantation.
Acknowledgements
No acknowledgement found.References
[1] Harris KM, Spirito P, Maron MS, et al. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation. 2006;(3):216-225.
[2] Kubo T, Gimeno JR, Bahl A, et al. Prevalence, clinical significance, and genetic basis of hypertrophic cardiomyopathy with restrictive phenotype. J Am Coll Cardiol. 2007;49(25):2419-2426.
[3] Biagini E, Spirito P, Rocchi G, et al. Prognostic implications of the Doppler restrictive filling pattern in hypertrophic cardiomyopathy. Am J Cardiol. 2009;104(12):1727-1731.
[4] Weng Z, Yao J, Chan RH, He J, Yang X, Zhou Y, He Y. Prognostic Value of LGE-CMR in HCM: A Meta-Analysis. JACC Cardiovasc Imaging. 2016. pii: S1936-878X(16)30406-5. [Epub ahead of print]
[5] Maron BJ, Spirito P. Implications of left ventricular remodeling in hypertrophic cardiomyopathy. Am J Cardiol. 1998;81(11):1339-44.
[6] Harris KM, Spirito P, Maron MS, et al. Prevalence, clinical profile, and significance of left ventricular remodeling in the end-stage phase of hypertrophic cardiomyopathy. Circulation. 2006;114(3):216-225.
[7] Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med. 2003;349(11): 1027-1035.
[8] Olivotto I, Cecchi F, Casey SA, Dolara A, Traverse JH, Maron BJ. Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001; 104(21):2517-2524.
Figures