2732
Free Breathing Myocardial MOLLI T1 Mapping using Real-time Slice Tracking and Non-Rigid Image Registration1Division of Imaging Sciences and Biomedical Engineering, King's College London, London, United Kingdom, 2MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom
Synopsis
The modified Look Locker (MOLLI) sequence is the most widely used myocardial T1 mapping approach. In this 2D sequence, several T1-weighted images are acquired within a breath hold and used to create a T1 map. However, some patients are unable to sustain stable breath-holds which generates 3D motion between the T1-weighted images. While image registration can potentially be used to correct for in-plane motion, through-plane motion cannot be corrected and may introduce bias in T1 estimates. In this study, we sought to develop and assess a free breathing MOLLI sequence with real-time slice tracking and non-rigid image registration to reduce in-plane and through-plane motion effects.
Purpose
Quantitative myocardial T1 mapping is a promising technique for the assessment of a variety of cardiomyopathies1. The modified Look Locker (MOLLI) sequence is the most widely used myocardial T1 mapping approach2. This 2D sequence acquires several T1-weighted images within a breath-hold. These images are then fit to a T1 recovery model to generate a T1 map. However, some patients are unable to sustain stable breath-holds which leads to in-plane and through-plane motion between T1-weighted images3,4. While image registration can potentially be used to correct for in-plane motion3,4, through-plane motion cannot be corrected retrospectively in such 2D acquisition and may introduce bias in T1 estimates. Therefore, the current MOLLI sequence may not be ideal for such patients. In this study, we sought to develop and assess a free breathing MOLLI sequence with real-time slice tracking and non-rigid image registration to reduce in-plane and through-plane motion effects.Methods
Proposed sequence: A prototype MOLLI sequence was developed by adding a navigator restore pulse after each inversion pulse and a navigator echo readout before each image acquisition. Real-time slice tracking was implemented based on the navigator echo and a tracking factor of 0.6 to reduce through-plane motion. Non-rigid image registration was performed online after acquisition to reduce in-plane motion. T1 fitting was performed using the conventional approach for MOLLI (3-parameter model fit followed by Look Locker correction5).
Experimental validation: All imaging was performed using a 1.5T Magnetom Aera scanner (Siemens Healthcare, Erlangen, Germany). All MOLLI T1 mapping scans used a bSSFP readout (TR/TE=2.5ms/1.2ms, flip angle=35°, FOV=360×306mm2, voxel size=2.2×2.5mm2, slice thickness=8mm, slice number=3, bandwidth=1085Hz/Px, GRAPPA acceleration factor=2, partial Fourier=0.87, MOLLI scheme: 5-(3)-3). The MR-navigator was positioned on the dome of the diaphragm of each subject.
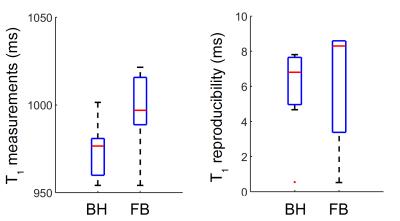
Study #1: Assessment of T1 mapping reproducibility. N=6 volunteers were recruited for a cardiac MRI study. Each volunteer was imaged twice using the conventional breath-hold (BH) MOLLI sequence and twice using the proposed free breathing (FB) MOLLI sequence. Both BH and FB sequences used the same imaging parameters described above. Native myocardial T1 measurements and reproducibility (absolute T1 time difference between the two scan repetitions) were evaluated. Both metrics were calculated for each of the 16 AHA myocardial segments as well as over all myocardial segments.
Study #2: Clinical feasibility. Three patients referred for assessment of cardiomyopathies were recruited. The feasibility of FB MOLLI was demonstrated in 3 patients referred to CMR for assessment of cardiomyopathy. Each patient was imaged using both BH and FB MOLLI sequences.
Results
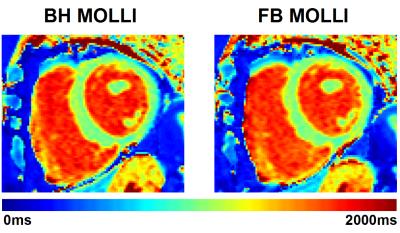
Study #1: Figure 1 shows representative native T1 maps acquired in one healthy volunteer using both the conventional (BH) and proposed (FB) MOLLI techniques. Excellent and similar image quality was obtained with both techniques. Figure 2 shows native myocardial T1 measurements and reproducibility obtained over all subjects. In average over all myocardial segments, native myocardial T1 times were 995±24ms using FB MOLLI and 974±16ms using BH MOLLI (p=0.01). There was no statistical significant differences between both techniques in terms of myocardial T1 reproducibility when measured in averaged over all myocardial segments (8±8ms using FB MOLLI vs. 8±7ms using BH MOLLI, p=0.46). There was no statistical differences between both techniques in terms of myocardial T1 reproducibility per myocardial segment (23±8ms using FB MOLLI vs. 18±6ms using BH MOLLI, p=0.22).
Study #2: Figure 3 shows representative native T1 maps obtained in one patient. Both conventional BH and proposed FB MOLLI sequences provided excellent and similar T1 map quality.
Discussion
The proposed FB MOLLI sequence was successfully applied in all tested cases, provided excellent myocardial T1 map quality, and similar reproducibility as the conventional BH MOLLI approach. Although real-time slice tracking was found successful in all subjects, the optimal tracking factor is subject-dependent and could occasionally lead to suboptimal tracking. Furthermore, the application of navigator pulses could potentially lead to blood signal tagging and blood T1 errors and will need to be carefully investigated in future studies.Conclusions
The proposed FB MOLLI sequence provides similar quality and reproducibility as the conventional BH MOLLI sequence. This sequence may represent a valuable alternative T1 mapping approach for patients unable to hold their breath.Acknowledgements
This research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre award to Guy's and St Thomas' NHS Foundation Trust in partnership with King's College London, and by the NIHR Healthcare Technology Co-operative for Cardiovascular Disease at Guy’s and St Thomas’ NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.References
[1] Moon JC, et al., Myocardial T1 mapping and extracellular volume quantification. J Cardiovasc Magn Reson 2013;15(1):92
[2] Messroghli DR, et al., Modified Look-Locker inversion recovery (MOLLI) for high-resolution T1 mapping of the heart. Magn Reson Med 2004;52(1):141–146
[3] Xue H, et al., Motion correction for myocardial T1 mapping using image registration with synthetic image estimation. Magn Reson Med, 2012;67(6):1644-1655
[4] Roujol S, et al., Adaptive registration of varying contrast-weighted images for improved tissue characterization (ARCTIC): Application to T1 mapping. Magn Reson Med, 2015; 73(4):1469-1482
[5] Deichmann R, Haase A. Quantification of T1 values by SNAPSHOT-FLASH NMR imaging. J Magn Reson, 1992;96(3):608–612.
Figures