2728
Association between cardiac iron clereance and hepatic siderosis by T2* MRI in thalassemia major patients1CMR Unit, Fondazione G. Monasterio CNR-Regione Toscana, Pisa, Italy, 2Azienda Ospedaliero-Universitaria Ospedali Riuniti "Umberto I-Lancisi-Salesi", Ancona, Italy, 3Fondazione di Ricerca e Cura "Giovanni Paolo II", Campobasso, Italy, 4Ospedale Sandro Pertini, Roma, Italy, 5Policlinico S. Orsola "L. e A. Seragnoli", Bologna, Italy, 6Policlinico Umberto 1, Roma, Italy
Synopsis
We evaluated in thalassemia major (TM) if the cardiac efficacy of the three iron chelators (Desferrioxamine, Deferiprone, and Deferasirox) was influenced by hepatic iron levels over a follow up of 18 months. In patients treated with Deferasirox and Deferiprone percentage changes in cardiac R2* over 18 months were associated with final liver iron concentration (LIC) and percentage LIC changes. In no chelation group percentage changes in cardiac R2* were influenced by initial LIC or initial cardiac R2*.
Purpose
The aim of this multicenter study was to evaluate in thalassemia major (TM) if the cardiac efficacy of the three iron chelators in monotherapy was influenced by hepatic iron levels over a follow up of 18 months.Methods
We evaluated prospectively the 98 TM patients enrolled in the MIOT Network1 who had been received one chelator alone between the two Magnetic resonance Imaging (MRI) scans and who showed evidence of cardiac iron (T2*<20 ms) at the basal MRI. Iron overload (IO) was measured by T2* multiecho technique.2 We used cardiac R2* (equal to 1000/T2*) because cardiac R2* is linearly proportional to cardiac iron and hepatic T2* values were converted into liver iron concentration (LIC) values.3Results
We identified 3 groups of patients: 47 treated with deferasirox (DFX), 11 treated with deferiprone (DFP) and 40 treated with desferrioxamine (DFO).
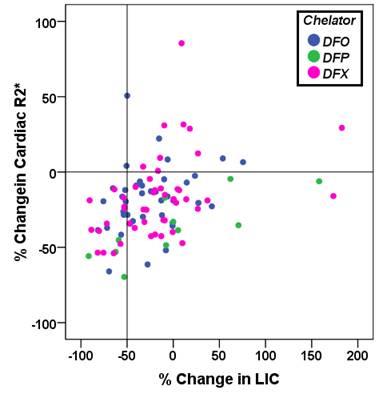
Percentage changes in cardiac R2* values correlated with changes in LIC in both DFX (R=0.469; P=0.001) and DFP (R=0.775; P=0.007) groups. All patients in these two groups who lowered their LIC by more than 50% improved their cardiac iron (see Figure 1). Percentage changes in cardiac R2* were linearly associated to the log of final LIC values in both DFX (R=0.437; P=0.002) and DFP groups (R=0.909; P<0.0001). Percentage changes in cardiac R2* were not predicted by initial cardiac R2* and LIC values.
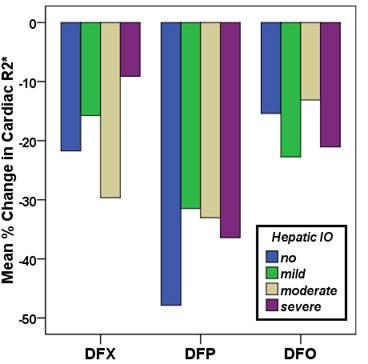
In each chelation group patients were divided in subgroups according to the severity of baseline hepatic iron overload (no, mild, moderate, and severe IO). The changes in cardiac R2* were comparable among subgroups (Figure 2).
Conclusions
In patients treated with DFX and DFP percentage changes in cardiac R2* over 18 months were associated with final LIC and percentage LIC changes.
In no chelation group percentage changes in cardiac R2* were influenced by initial LIC or initial cardiac R2*.
Acknowledgements
No acknowledgement found.References
1. Meloni A, Ramazzotti A, Positano V, et al. Evaluation of a web-based network for reproducible T2* MRI assessment of iron overload in thalassemia. Int J Med Inform. 2009;78(8):503-512.
2. Pepe A, Positano V, Santarelli F, et al. Multislice multiecho T2* cardiovascular magnetic resonance for detection of the heterogeneous distribution of myocardial iron overload. J Magn Reson Imaging. 2006;23(5):662-668.
3. Meloni A, Rienhoff HY, Jr., Jones A, et al. The use of appropriate calibration curves corrects for systematic differences in liver R2* values measured using different software packages. Br J Haematol. 2013;161(6):888-891.