2721
Towards High Success Rate in vivo Cardiac DTI on a Clinical 3T Scanner: Considerations on Heart Rate, Body-to-Mass Index, and Free Breathing1Biomedical Imaging Research Institute, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 2Bioengineering, University of California Los Angeles, Los Angeles, CA, United States, 3Siemens Healthcare, Los Angeles, CA, United States
Synopsis
Clinical translation of cardiac diffusion tensor MRI has been challenging because of the sensitivity to bulk motion and thus, low success rates of scans. Current techniques require either high gradient systems (>40 mT/m) or excess breath holding ( >10 breath holds / slice) to acquire motion free cardiac DT-MRI. We propose a cardiac DT-MRI technique optimized for clinical translation and aimed at achieving high success rates in subjects with high and variable heart rate and high bold-to-mass index under free breathing conditions. Results in subjects with high BMI and variable HR yielded success rates > 90%.
INTRODUCTION
Cardiac diffusion tensor MRI (DT-MRI) is a powerful, non-invasive technique capable of mapping fiber architecture and yield new insight to myocardial tissue microstructure1-3. Translating cardiac DT-MRI to the clinic has continued to be challenging due to the inherent sensitivity to bulk motion and long scan times. Significant advances have been made using free breathing second order motion compensation (M2) via gradient moment nulling spin echo, but success rates in acquiring bulk motion artifact free images remain insufficient for routine clinical use. We propose a cardiac DT-MRI technique optimized for clinical use at 3T that could address typical patient characteristics such as varying/high heart rate (HR), high body-to-mass index (BMI), and difficulty in performing breath holds.METHODS
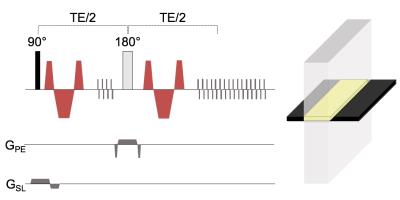
PULSE SEQUENCE DESIGN: The proposed DT-MRI technique uses an optimized M2 spin echo1 reduced field-of-view (FOV) single shot echo-planar-imaging (EPI) (Figure 1). M2 spin echo diffusion encoding was used to address both cardiac and respiratory bulk motion with regard to diffusion motion sensitivity leading to possible signal drop out. ECG gating at end systole was prescribed to address variable HR and retrospective non-rigid motion correction (MIRT4) to address respiratory motion shifts between diffusion weighted directions and averages during free breathing acquisition (Figure 2). Reduced FOV EPI via cross-pair spin echo addresses high BMI with only the heart being selectively imaged instead of the entire FOV. Additionally, EPI at high field (≥3T) is prone to the increased main field inhomogeneity and requires a short readout to avoid severe susceptibility artifacts and geometric distortion5. Both partial (5/8) Fourier in the phase encode and reduced field-of-view (FOV; 33%) was used to reduce the EPI echo train by a factor ~5.
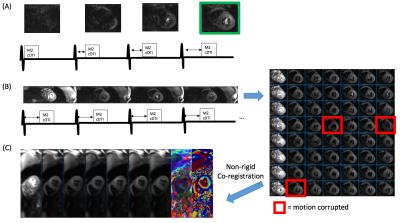
IN VIVO IMAGING: Eight (n = 8) volunteers without any history of cardiovascular disease but exhibited variable HR during DT-MRI scan (SD: 12 +/- 3 beats-per-minute (BPM); Range: [58 95] BPM) and high BMI (30 +/- 4.5, [25 – 36]) were scanned using the proposed free breathing M2 DT-MRI sequence (TR=4RR, TE=85ms, EPI temporal footprint = 15ms, 3 short axis, 2.3x2.3x10mm, 1b0 + 6 directions, 8 averages, scan time: 2.5 min) on a clinical wide bore (70cm) 3T scanner (Skyra, Siemens Healthcare, Erlangen, Germany). A scout mode that continuously acquired a single DWI at varying trigger delays preceded the DT-MRI scan (Figure 2a). Once a trigger was quickly found yielding motion free images, then that trigger was used for the entire DT-MRI scans for all averages and directions.
IMAGE ANALYSIS: Diffusion tensors were fitted voxelwise after non-rigid co-registration was applied to correct respiratory motion assuming a mono-exponential fit using custom software developed in Matlab. Mean diffusivity (MD), fractional anisotropy (FA), and helix angle (HA) were calculated from the reconstructed tensor. Success rates were determined by the number of DWI that did not exhibit greater > 10% signal loss (apparent diffusion coefficient > 3.0 um^2/ms; labeled as “motion corrupted” in figure 2c) out of all DWI acquired (6 directions x 8 averages = 48). Success rates were plotted against HR, HR variability (standard deviation of HR during scan), BMI, and age.
RESULTS
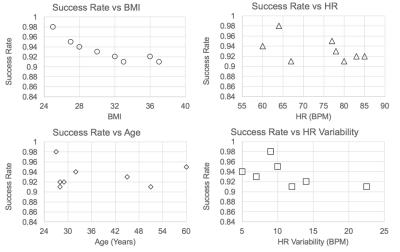
Success rates (93% +/- 2%) of cardiac DT-MRI scans were high across all BMI, HR, HR variability, and ages (Figure 3). Low correlation (R^2 < 0.3) was found between success rate and HR, HR variability, and age. Substantial correlation (R^2 = 0.8) was found between success rate and BMI, although the slope of the fitted line was appreciably small (0.0045 success rate / BMI). Mean MD (1.4 +/- 0.2 um2/ms), FA (0.32 +/- 0.1), and HA (-1.2 +/- 0.2 degrees/%transmural depth) were within range of normal volunteers previously reported in literature2,3.DISCUSSION
Cardiac DT-MRI currently has low success rates when HR, HR variability, and BMI are high. Clinical application of cardiac DT-MRI requires high success rates in patients who typically have high HR, HR variability, and BMI. Additionally, free breathing is a desirable feature for clinical imaging especially since cardiac DT-MRI requires long scan times (10-15 minutes) for full LV coverage). The proposed cardiac DT-MRI technique demonstrated high success rates (>90%) defined by the fraction of motion-free artifacts can be achieved regardless of high BMI, HR, and HR variable on a clinical 3T scanner.CONCLUSION
A novel cardiac DT-MRI was developed to include robust end systolic imaging, reduced FOV, and image-based motion correction to address high/variable HR, high BMI, and free breathing, respectively. These developments led to a high success rate cardiac DT-MRI technique capable of imaging on a wide bore clinical 3T system. Clinical studies using this novel technique are needed to completely test the robustness in patients.Acknowledgements
No acknowledgement found.References
1. Nguyen C, Fan Z, Xie Y, Pang J, Speier P, Bi X, Kobashigawa J, Li D. In vivo diffusion-tensor MRI of the human heart on a 3 tesla clinical scanner: An optimized second order (M2) motion compensated diffusion-preparation approach. Magn. Reson. Med. 2016 Aug 1.
2. Mekkaoui C, Reese TG, Jackowski MP, Bhat H, Sosnovik DE. Diffusion MRI in the heart. NMR Biomed. 2015 Oct 20.
3. Stoeck CT, Deuster von C, Genet M, Atkinson D, Kozerke S. Second-order motion-compensated spin echo diffusion tensor imaging of the human heart. Magn. Reson. Med. 2015 May 28.
4. Myronenko A, Song X. Intensity-based image registration by minimizing residual complexity. IEEE Trans. Med. Imaging. 2010 Nov;29(11):1882–91.
Figures