2675
Detailing and Enhancing Respiratory Motion Induced Myocardial B0 Field Dispersion at 7.0 T: Implications for Cardiac Imaging and Spectroscopy at Ultrahigh Magnetic Field Strengths1Berlin Ultrahigh Field Facility (B.U.F.F.), Max Delbrück Center for Molecular Medicine in the Helmholtz Association(MDC), Berlin, Germany, 2Physikalisch Technische Bundesanstalt (PTB), Berlin, Germany, 3Experimental and Clinical Research Center, a joint cooperation between the, Charité Medical Faculty and the Max Delbrück Center for Molecular Medicine in the Helmholtz Association, Berlin, Germany, 4DZHK (German Centre for Cardiovascular Research), partner site Berlin, Berlin, Germany
Synopsis
Respiratory motion induced B0 field fluctuations, constitute a challenge for B0 sensitive CMR like spectroscopy. Accommodating CMRS in a single breath-hold is elusive if not prohibitive. Motion corrected approaches under free breathing were demonstrated to substantially improve CMRS. Yet, B0 field fluctuations over the respiratory cycle may compromise spectral resolution and data integrity. A compensation strategy like dynamically updated first order shims synchronized with the respiratory motion, offers the potential to enhance spectral quality and permits scan time shortening. This work details respiratory motion induced B0 fluctuations in the interventricular septum and examines the capability of linear shimming for compensation of myocardial B0 fluctuations.
Purpose
Cardiac magnetic resonance 1H spectroscopy (CMRS) provides means for probing myocardial energy metabolism for the study of cardiac disease and heart failure [1]. The heart is one of the more challenging target organs for MR due to cardiac and respiratory motion. Cardiac motion has only very minor impact on B0 field homogeneity in the interventricular septum and its fluctuation throughout the cardiac cycle [2]. Unlike cardiac motion, respiratory motion induced B0 field fluctuations [3] constitute a challenge for B0 sensitive CMR. In cardiac MRI this issue is commonly dealt with by breath hold techniques. Accommodating CMRS in a single breath-hold is elusive if not prohibitive. CMRS may benefit from free-breathing approaches, which – if properly motion corrected – were demonstrated to substantially improve CMRS [4]. Yet, B0 field fluctuations over the respiratory cycle may compromise spectral resolution and data integrity. A compensation strategy like dynamically updated first order shims [5, 6] synchronized with the respiratory motion, offers the potential to enhance spectral quality and permits scan time shortening. This work details respiratory motion induced B0 fluctuations in the interventricular septum and examines the capability of linear shimming for compensation of myocardial B0 fluctuations.Methods
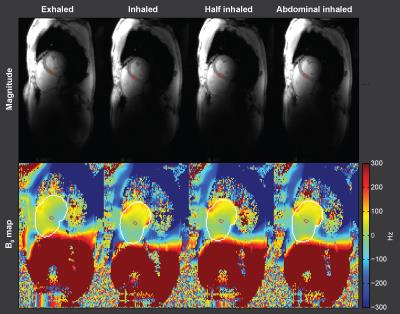
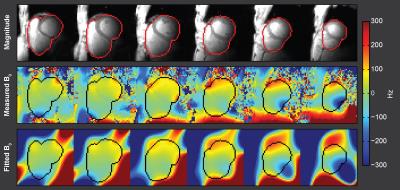
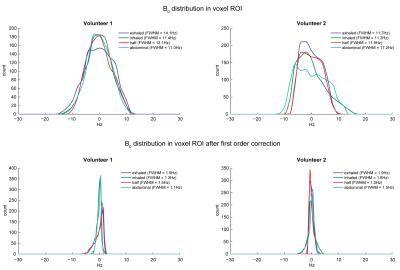
Two healthy volunteers of different body type (1 male, muscular, age=33, BMI=25.5 kg/m2, 1 female, slender, age=37, BMI=18.8 kg/m2) were examined prior to lunch using a 7.0T whole body MR system (Siemens Healthcare,Erlangen,Germany) using a 16 channel RF-transceiver array for signal transmission and reception [7]. B0 mapping was performed with a cardiac triggered double echo gradient echo technique (TE=(2.04, 4.08)ms, TR=5.9ms, spatial resolution=(2.8x2.4x4.0)mm3), GRAPPA R=2, 8 slices covering the whole heart, gap=8mm). Volume selective shimming was applied for a volume accommodating the heart, based on an end diastolic cardiac triggered field map (TE=(2.04, 4.08)ms, TR=5.4 ms, spatial resolution (4.2x4.2x8.0)mm3, 18 slices, gap=1.6mm). A polynomial fit of 5th order was applied to the measured field map to approximate B0 and allow evaluation in arbitrary volumes at high spatial resolution. The fit was evaluated on a 1mm3 isotropic grid. B0 homogeneity was investigated for four breathing positions (diaphragmatic exhaled, diaphragmatic inhaled, diaphragmatic half-inhaled, abdominal-inhaled) using a mid-septal ROI resembling a spectroscopic voxel of size (18.7x9.4x6.1)mm3 [4] (Fig.1). Histograms of the field distribution in the ROI were calculated. Prior to this the mean B0 value within the ROI was subtracted for easier comparison of the histograms. The histogram full width half maximum (FWHM) was calculated as a measure of field homogeneity. The effect of a shim of first order was simulated to investigate it’s capability to correct for field inhomogeneities by applying a linear fit to the approximated field in the ROI and subtracting it from the fitted field map. B0 homogeneity after this virtual shim was again assessed using histograms of the field distribution within the ROI.Results
The fitted field maps closely approximated the measured field maps (Fig.2). Overall field homogeneity was comparable for both volunteers. The mean B0 dispersions across the myocardial voxel were FWHM= (12.9±1.6)Hz, (11.3±0.1)Hz, (12.0±0.1)Hz and (14.1±4.4)Hz (mean±std) for the diaphragmatic (exhaled, inhaled, half-inhaled) and abdominal-inhaled positions (Fig.3). While field homogeneity was best for the abdominal breath hold and worst in the exhaled state in volunteer 1 (FWHM=11.0Hz and 14.1Hz), it was best in the exhaled state and worst during the abdominal breath hold in volunteer 2 (FWHM=11.7Hz and 17.2Hz). The deviation in homogeneity between the two subjects was highest for the abdominal breath hold (ΔFWHM=6.2Hz). After applying the linear field correction the mean B0 dispersion across the septal voxel was substantially improved to FWHM=(1.9±0.0)Hz, (1.5±0.2)Hz, (1.3±0.3)Hz and (1.3±0.2)Hz (Fig.3), with abdominal and half-inhaled positions yielding the highest field homogeneity for volunteer 1 and 2 respectively (FWHM=1.1Hz and 1.2Hz).Discussion and Conclusion
Our results show that respiration affects myocardial B0 dispersion, which is prone to thorax geometry and breathing state. Our findings demonstrate that first order field correction substantially improves field homogeneity across a small target volume and permits a B0 fidelity of FWHM≈1Hz. Our results provide encouragement for free breathing myocardial spectroscopy at 7.0 Tesla. To take it to the next level we will evaluate how the myocardial B0 homogeneity outside the ROI might be compromised by the linear shim, and how B0 non-uniformities in the vicinity of the ROI may influence cardiac 1H MRS [8].Acknowledgements
No acknowledgement found.References
[1] Ewijk et al. (2015) NMR Biomed 28(7):747. [2] Huelnhagen et al. (2016) Magn Reson Med, Epub ahead of print, doi:10.1002/mrm.26312. [3] Schmitter et al. (2015) Magn Reson Med 74(5):1291. [4] Fillmer et al., Proc. Intl. Soc. Magn. Reson. Med. 24, 2016:1100. [5] Blamire et al. (1996) Magn Reson Med 36(1):159. Fillmer et al. (2015) Magn Reson Med 75(3):1119. [7] Thalhammer et al. (2012) J Magn Reson Imaging 36(4):847. [8] Fillmer et al. (2015) Magn Reson Med 73(4):1370.Figures