2640
An investigation of skin/skin contact RF burns1Toshiba Medical Research Institute, Mayfield Village, OH, United States
Synopsis
Third degree RF burns at skin/skin contact points have been reported. A thermal dose injury mechanism is widely assumed and thermal modeling results based on a well-documented calf burn report are presented. A hotspot ratio (Local:Whole Body SAR) of 86 results in various arbitrary CEM43 defined thresholds being exceeded after a few minutes of inadvertent skin/skin contact. The results support the hypothesis that skin/skin contact thermal injury burns are possible after several minutes of routine clinical scanning.
Purpose
To understand anticipated levels of ohmic heating in skin/skin contact burn cases which may provide insight on appropriate RF power limits and clarify the need for preventive measures.Methods
Skin/skin burns are likely the result of local ohmic heating. The heating is the result of RF induced eddy currents over large areas channeled through a local restriction, such as a skin/skin point contact. This is fully modelled (Sim4Life, ZMT, Switzerland).
A third degree burn at the point of touching calves has been well documented [1] with a maximum SAR of ~1 W/kg (all sequences used, except one, were Spin Echo) and a total examination time of 53 minutes. The target imaging region was mid-thigh and the point of skin/skin contact was mid-calf.
The details of the whole body coil transmit coil in [1] are unknown. These simulations are based on ISO/TS10974 and are previously used [2, 3]: 16-rung high-pass birdcage coil, d=750mm, l=650mm. RF shield: d=790mm, l=850mm. The transmit coil end ring location in [1] is unknown but is close to skin/skin contact point for the end rings used in the modeling presented here.
Thermal dose results are computed by CEM43 [4]. Duke modelling started at an initial 37oC but two hours provided to reach thermal equilibrium (35.9oC) before start of scanning.
Results
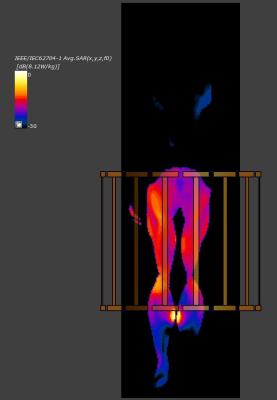
Figure 1 shows SAR (1.5T) in Duke [5] in the coronal plane at the level of highest SAR (local: 8.12 W/kg, Whole Body: 0.094 W/kg, for a hotspot ratio: 86.4. Nominal B1+rms field central axial slice average: 1.1 μT).
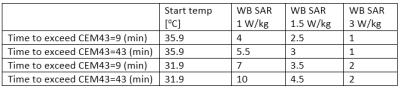
Tissue damage is a function of thermal dose [7]. Skin burns have been reported as low as CEM43=43 [6], but [7] proposes a general cautionary limit of CEM43=9. Table 1 lists the time to exceed the two thresholds, all assuming normal perfusion values and a starting skin temperature of ~36oC. A stable temperature of ~53oC is reached in ~22 minutes for the 1 W/kg condition, and the same temperature is reached in ~4.5 minutes at 1.5 W/kg, ~1.5 minutes at 3 W/kg. The respective steady state temperatures for the three cases: ~53oC, ~62oC, ~84oC respectively. The starting skin temperature is ~4oC higher compared to typical, in which case the three pairs of CEM43 time would be longer, as also shown in Table 1.
Discussion
The WB SAR exposure in [1] was 1 W/kg. Given MR vendors typically over-report SAR to comply strictly with IEC 60601-2-33 limits, true SAR was probably lower. Additionally, IEC 60601-2-33 provides a “partial body” SAR control that scales as a fraction of the total body mass receiving 95% of all RF power. For this particular landmark/model/RF coil combination, the maximum permitted SAR, expressed as a Whole Body equivalent, is 3 W/kg. However, it has been noted [3] that typical clinical usage may not reach the permitted limits. Since publication in 1996 [1], typical SAR exposures in an equivalent clinical situation may have increased up to 1.5 W/kg with the widespread adoption of FSE (TSE) sequences. The IEC short term 2x SAR exposure allowance is not applied unless standard limits are exceeded. In general, higher average whole body SAR exposures are expected at 3T with similar hotspot ratios.
The presented hotspot ratio of 86 exceeds the previously reported ~50 in the groin region during ankle scans [8], implying a maximum local SAR of ~258 W/kg at skin/skin contact at maximum permitted WB exposure.
It is unknown for how long the calves in [1] were actually touching. It is recognized [6] that the skin conductive characteristics can change significantly, nor is it known if the left/right leg girth asymmetry in [1] due to a prior surgical procedure is significant. Lastly, this is the modeling result for one single case and it is unknown how significantly such high hot-spot ratios may vary between models or how variations in perfusion characteristics will change final numeric results.