2634
Bilateral Breast Phantoms for Fusion to Human Voxel Models for Specific Absorption Rate (SAR) Simulations1Weldon School of Biomedical Engineering, Purdue University, West Lafayette, IN, United States, 2School of Electrical and Computer Engineering, Purdue University, West Lafayette, IN, United States
Synopsis
To comply with US Food and Drug Administration (FDA) guidelines of MRI safety, we propose a method to simulate Specific Absorption Rate (SAR) information with bilateral breast phantoms seamlessly integrated to a human model. This modeling method can be used with various breast phantoms. The simulation results indicate breasts with high glandular contents are more susceptible to SAR safety concerns compared to breasts with low glandular content.
Introduction
Breast cancer is one of the leading causes of death in United States. X-ray examination of breast cancer, also known as Mammograms, have been shown to give false negative result. 1 In addition, exposure to radiation can cause further tissue damage. Therefore, MRI has been used an alternative breast cancer examination because it provides more detailed tissue structure, and is free of ionizing radiation. One of the major concerns in MRI exam is the Specific Absorption Rate (SAR) which can cause elevated temperature in tissue due to RF power deposition. To comply with US Food and Drug Administration (FDA) guidelines of SAR maximum 8 W/kg for 15 minutes for any gram of tissue in torso, 2 we propose a method of simulation in a full-wave simulation software (XFdtd, Remcom, State College, PA, USA) of SAR information in the breast phantom which is seamlessly integrated to a human model in the 7T RF environment.Method
A novel modeling method using MATLAB (The MathWorks Inc., Natick, MA, USA) is proposed to allow integration of heterogeneous breast phantoms on the pectoral muscle wall of human model. For this work, we adapted four 0.5-mm resolution breast phantoms from Hagness’ group at the University of Wisconsin–Madison (UW) 3 and one female whole-body model “Ella” from Virtual Population. 4 Torso pectoral muscle wall are first extracted from the human phantom. A series of morphological operations are performed on the pectoral muscle wall to smooth the surface. Using affine transformation of 1D axial array of breast phantoms based on the translation parameters from the contours of the pectoral muscle 3D projection, breast phantoms are integrated to human voxel model. Physical and electrical properties are assigned to different tissue types of the phantom based on IT’IS Foundation database. 5 A previously reported quadrature volume RF coil, driven by 298-MHz sinusoidal feeds with 90-degree phase shift, is used to generate the electromagnetic field. 6 The net input power for the simulation is set to 1 W.Result
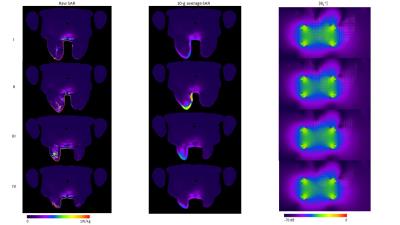
Figure 1 shows the breast phantom after modification. A muscular layer was added to the bottom of the breast phantom before aligning it to pectoral muscle. Figure 2 shows the seamless integration of breast with patient in the prone position. The coil does not touch any part of the body, and there is enough spacing between the breast and coil. Figure 3 shows the raw SAR, 10-g average SAR and |B1+| in the axial plane of 4 heterogeneous breast phantoms: (I) almost entirely fat, (II) scattered fibroglandular tissue, (III) heterogeneous fibroglandular tissue, and (IV) extreme fibroglandular tissue. The raw SAR plots display localized maximum regions in tissues with high conductivity and relative permittivity. The 10-gram spatial average SAR plots reveal whether maximum 10-g average SAR incorporates with the gland or muscle regions interior to the breast or skin layer at the breast surface. The |B1+| field shows the distribution of the transmit field in the axial plane of the breast phantoms. The breast phantoms are outlined as dotted lines in the |B1+| plots.Discussion
As shown in the raw SAR plots, the skin, fibro-connective tissues and pectoral muscle incorporate local maximum SAR, because they have high relative permittivity and electrical conductivity at the 7T Larmor frequency. Notably, maximum 10-g average SAR incorporates with skin layer at the breast surface in all 4 breast phantoms. That is because breast skin layers are close to the excitation fields source and the excitation fields firstly attenuate within the skin layers. The homogeneity of |B1+| field inside the breast indicates the breast phantoms are homogeneously excited. The breast morphology and size in the |B1+| field also affects the SAR distribution within the breast phantom; this can be seen in IV breast phantom, where less SAR incorporates with glandular and skin contents due to non-rounded breast shape and small breast size as compared to III.Conclusion
As demonstrated, this modeling method can be used with various breast phantoms. Breasts with high glandular contents are more susceptible to SAR safety concerns as compared to breasts with low glandular content. In future work, we will conduct thermal simulations and add more variations in human voxel models.Acknowledgements
No acknowledgement found.References
1. Wallis, M. G., Walsh, M. T., & Lee, J. R. (1991). A review of false negative mammography in a symptomatic population. Clinical radiology, 44(1), 13-15.
2. Center for Devices and Radiological Health, Food and Drug Administration (1998) Guidance for the submission of premarket notifications for magnetic resonance diagnostic devices. Rockville, Maryland.
3. Zastrow E, Davis SK, Lazebnik M, Kelcz F, Van Veen BD, Hagness SC (2008) Development of anatomically realistic numerical breast phantoms with accurate dielectric properties for modeling microwave interactions with the human breast. IEEE T Bio-Med Eng 55:2792-2800. doi: 10.1109/TBME.2008.2002130.
4. Christ A, Kainz W, Hahn EG, Honegger K, Zefferer M, Neufeld E, Rascher W, Janka R, Bautz W, Chen J, Kiefer B, Schmitt P, Hollenbach H-P, Shen J, Oberle M, Szczerba D, Kam A, Guag JW, Kuster N (2010) The Virtual Family—development of surface-based anatomical models of two adults and two children for dosimetric simulations. Phys Med Biol 55:N23-N38. doi: 10.1088/0031-9155/55/2/N01.
5. Hasgall P, Neufeld E, Gosselin M, Klingenböck A, Kuster N (2013) IT’IS database for thermal and electromagnetic parameters of biological tissues. IT’IS Foundation. http:// www.itis.ethz.ch/database.
6. McDougall MP, Cheshkov S, Rispoli J, Malloy C, Dimitrov I, Wright SM (2014) Quadrature transmit coil for breast imaging at 7 tesla using forced current excitation for improved homogeneity. J Magn Reson Imaging 40:1165-1173. doi: 10.1002/jmri.24473.
Figures