2617
Treatment for Spontaneous Intracranial Hypotension: First Experience with MRI Guided Percutaneous Blood Patch and Fibrin Injection.1Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University School of Medicine, Baltimore, MD, United States
Synopsis
MRI guided blood patch/fibrin injection (BFP) instead of CT BFP as treatment option for SIH, first case reported. Avoids radiation exposure, helpful for adolescents and women in reproductive age. Obviates CT myelography, decreasing risks, time, and making it available for patients with iodine allergy. Our case is a 26 yo female with SIH. Axial PD, Axial and Sagittal T2 HASTE were used for localization of dural ectasia. T2 HASTE MRI fluoroscopy was used for spinal needle placement at the T12-L1 epidural space and injection of 10cc autologous blood and 2 cc of fibrin. The result was improvement of symptoms.
Purpose
Spontaneous Intracranial Hypotension (SIH) refers to decrease in the intracranial pressure accompanied by clinical symptoms, most commonly postural headache. The suggested pathology is leaking of the CSF from a dural tear1. The incidence is 5 per 100 000 at any age, even among adolescents, but is most frequently recorded among females in late middle age 2. There are a variety of therapeutic options including conservative therapy, surgery, non-targeted and image guided blood patch and fibrin injection 3-4. Many studies favored CT guided epidural blood/fibrin patch, because it is minimally invasive, ambulatory and without the inherent risks of an open surgery 5. The drawbacks are the need to perform a myelogram to delineate the areas of CSF leak, and the radiation. MRI guided percutaneous epidural blood patch/fibrin injection (BFP), is theoretically an excellent alternative because it: 1) Allows real-time anatomic visualization of CSF spaces without an intrathecal injection, defining contours of dural diverticula allowing for better epidural targeting, and 2) avoids radiation from the procedure which is desirable in young women of childbearing age.Methods
Patient: 26 yo female with Chiari malformation status post decompressive surgery (2011). The headaches present almost every day, and usually occur in the back, right side of her head. Pain level 4-5/10, improves when lying down. Opening Pressure 9cm of H20.
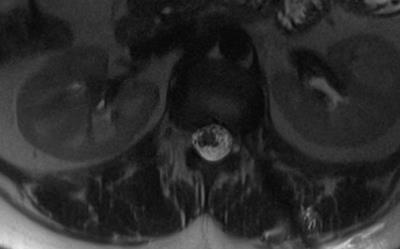
Pre procedure MRI: Informed consent was obtained and details about the risks and benefits of the procedure were discussed with the patient. The patient was positioned prone in a clinical wide-bore 3 Tesla MR imaging system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). Axial intermediate-weighted TSE images extending from from T8 – L2 localized the area of dural ectasia at T12-L1 on the left. Dedicated axial and sagittal T2-weighted HASTE TSE images were obtained for confirmation (Figure 1).
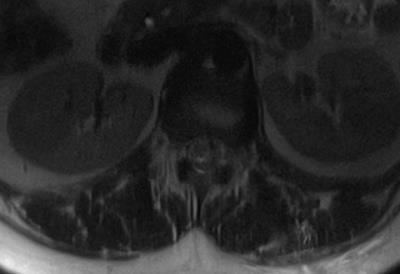
Procedure and Intraprocedural MRI: The area of dural ectasia at T12-L1 on the left was targeted using the integrated position laser of the system and skin markers. Utilizing real-time T2-weighted HASTE TSE MRI fluoroscopy, a 3.5 inch 20-gauge MRI compatible spinal needle was advanced into the left lateral epidural space at T12-L1 adjacent to the area of dural ectasia (Figure 2). After confirmation of needle placement, 10 mL of autologous blood was injected into the epidural space, which was followed by 2 mL of fibrin. Axial and sagittal T2 HASTE images, as well as axial intermediate-weighted TSE images were utilized to evaluate the epidural space and the mass effect over the thecal sac (Figure 3). Post Procedure: Axial T1 and axial and sagittal T2-weighted TSE images confirmed satisfactory epidural blood and fibrin patch.
Results
Real time MRI fluoroscopy showed distribution of the autologous blood and fibrin in the epidural space at the level of T12-L1, with extension through the epidural space. No immediate complications were identified. The patient was admitted over night for evaluation by our Neurosurgery service. Outpatient follow-up 1 month after the procedure confirmed decrease in headache frequency to 2 headaches in 5 weeks, and pain scale raging from 0-6/10. Patient referred “feels clearer and more normal” and “my brain fog has gone”. Patient experienced rebound CSF hypertension managed with acetazolamide 250 mg PO BID.Discussion
Blood/Fibrin patch is a recognized minimally invasive therapy for treatment of spontaneous intracranial hypotension. Utilizing MRI for BFP instead of CT avoids radiation exposure of approximately 10-30 mSV 6-7, which is especially helpful for adolescents and women in reproductive age. Studies comparing CT myelogram and MRI myelogram show great correlation in defining the anatomy of treatment targets 8. MR imaging with heavily T2-weighted TSE images, allows visualization of the thecal sac, dural diverticuli, and leaks. We believe CT myelography can be omitted, which reduces time, one additional dural puncture, and avoids the inherent risks of myelography, and is especially helpful for patients with iodine allergies. MR fluoroscopy also allows us to visualize the accurate location of the BFP in real time and gives immediate feedback during the procedure.Conclusions
To our knowledge, this is the first experience with MRI-guided BFP for treatment of SIH. The results are satisfactory and MRI guidance comes with the advantage of no exposure to ionizing radiation and no need of intrathecal contrast, which make this procedure an excellent alternative to current treatments options. Further studies are needed to evaluate the consistency and efficacy of this approach.Acknowledgements
No acknowledgement found.References
1. Gordon, N. (2009). Spontaneous intracranial hypotension. Developmental Medicine and Child Neurology, 51(12), 932-5).
2. Mea E, Chiapparini L, Savoiardo M, Franzini A, Bussone G, Leone M. Headache attributed to spontaneous intracranial hypotension. Neurol Sci 2008; 29: S164-5.
3. Kranz, P. G., L. Gray, and J. N. Taylor. "CT-guided epidural blood patching of directly observed or potential leak sites for the targeted treatment of spontaneous intracranial hypotension." American journal of neuroradiology 32.5 (2011): 832-838.
4. Gladstone, Jonathan P., et al. "Spontaneous CSF leak treated with percutaneous CT-guided fibrin glue." Neurology 64.10 (2005): 1818-1819.
5. Sencakova, Drahomira, Bahram Mokri, and Robyn L. McClelland. "The efficacy of epidural blood patch in spontaneous CSF leaks." Neurology 57.10 (2001): 1921-1923.
6. Kranz, Peter G., et al. "Myelographic techniques for the detection of spinal CSF leaks in spontaneous intracranial hypotension." American Journal of Roentgenology 206.1 (2016): 8-19.
7. Van Unnik, J. G., et al. "Survey of CT techniques and absorbed dose in various Dutch hospitals." The British journal of radiology 70.832 (1997): 367-371.
8. Wang, Y-F., et al. "Heavily T2-weighted MR myelography vs CT myelography in spontaneous intracranial hypotension." Neurology 73.22 (2009): 1892-1898.
Figures