2607
MRI-based Synthetic CT for Radiation Treatment of Lung Cancer1Department of Radiation Oncology, New York University School of Medicine, New York, NY, United States, 2Bernard and Irene Schwartz Center for Biomedical Imaging, Department of Radiology, New York University School of Medicine, New York, NY, United States, 3Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
With emerge of MR-linear accelerator technology, the interest for MR-only radiotherapy is growing rapidly. This study evaluated the feasibility of using pseudo-CT generated from conventional Dixon-MR scans for treatment planning of lung cancer where dosimetric differences are expected to be high due to tissue inhomogeneity. A model-based method including spine was applied to generate synCT from whole-body Dixon-MR data. The plans for radiotherapy in lung cancer calculated on synCT images closely agreed with the doses computed on standard CT to within 1%. Further evaluation of the MR-based treatment planning in a large patient cohort is needed.
Purpose
MR images are used currently to delineate tumors and organs at risks (OARs) in radiation oncology. An MR-only radiotherapy would reduce patient radiation, improve efficiency, and avoid the issues related to the alignment of MR images with CT scans1. However, MR signal does not provide electron-density required for dose calculation in radiation therapy. The purpose of this study was to evaluate the feasibility of MR-derived synthetic CT (synCT) for radiation treatment planning of lung cancer where inhomogeneity correction is critical component in dose calculation.Methods
Eleven patients who underwent whole-body PET/MR following PET/CT examination were randomly selected from an ongoing prospective IRB-approved study. The MR data was obtained on a 3 T whole-body system (Biograph mMR, Siemens Healthcare) using a 2-point, 3-dimensional volume-interpolated breath-hold Dixon-sequence (3.6 ms TR, 2.46 ms TE, 10o flip angle, 192 × 126 in-plane dimension and 128 slices in a coronal orientation). The CT was acquired according to a standard clinical protocol on a PET/CT scanner (Biograph mCT, Siemens AG Healthcare).
A previously published spine-included model-based method2 that generated linear attenuation coefficients for PET attenuation correction was employed to generate µ (mu) maps from the Dixon scans. The MR-generated µ maps were converted to provide synCT, assuming a conventional 100-140 kVp x-ray source. The synCT images were registered to CT images by using first rigid and then deformable registration in Velocity (Velocity AI 3.1.0, Velocity Medical Solutions, Altanta, GA). Both synCT and CT images were imported into the treatment planning software Eclipse (Eclipse 11.0.47; Varian Medical Systems, Palo Alto, CA) for treatment planning. Four sets of planning target volumes (PTVs) at apex, central, lower and posterior lobe with three tumor sizes (small, medium, and large-sized) were manually contoured in the lung and the density was overridden as water. Conventional or hypofractionated radiation treatments for the PTVs were planned on synCTs. The PTV, OARs, and plan were copied to the CT images. The plans were then recalculated on the CT volume using the same monitor unit (MU) as the synCT plan (Fig.1). Dose distributions between synCT and CT were compared using the global 3D gamma analysis3.
Results
The mean Hounsfield-unit (HU) differences (mean ± standard error) between synCT and CT were 2 ± 18, 2 ± 16, 2 ± 13, 19 ± 6, and -74 ± 25 for right lung, left lung, heart, spinal cord and spine bone, respectively. T-tests indicated that synCT has comparable mean CT numbers as conventional CT in the lung and soft tissues. Mean differences between PTV dose on synCT and CT across all the plans (Fig. 2) were -0.1% ± 0.4%, 0.1% ± 0.5%, and 0.4% ± 0.5% for D95 (percentage dose covering 95% PTV), D98 and D100, respectively and these differences were not statistically significant . Doses between two data sets for OARs had average differences of -0.14 ± 0.07 Gy, 0.0% ± 0.1%, and -0.1% ± 0.2% for the maximum spinal cord dose (Dmax), percentage of lung volume receiving 20Gy dose (V20), and percentage heart volume receiving 40Gy dose (V40), respectively. Gamma analysis (table I) revealed a passing rate of 99.3% ± 1.1% for 2%/2mm (dose difference/distance to agreement) acceptance criteria, suggesting good agreement between synCT and CT calculated doses.Conclusions
The synCT generated from Dixon-MR using a model-based method allows dose calculation equivalent to standard CT for lung cancer treatment planning. The dosimetric agreement between synCT and CT are comparable that warrants further development for MR-only workflow in radiation treatment planning.Acknowledgements
No acknowledgement found.References
1. Schmidt MA, et al. Physics in Medicine and Biology, 2015, 60: R323-361.
2. Paulus DH, et al. Journal of nuclear medicine, 2015, 56(7):1061-1066.
3. Low DA, et al. Medical physics 1998, 25(5):656-661.
Figures

1. Dose distribution on Synthetic CT and standard CT. PTVs of different sizes are contoured at different locations in the lung.
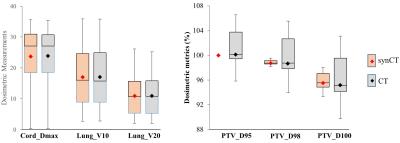
2. Dosimetric metrics in all the plans for OARs (left) and PTV (right). Total 43 tumors were simulated in 11 patients for treatment planning and dose comparisons. Error bar represent distribution from different patients.
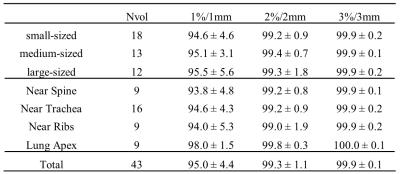
Table I. Means and standard deviations of gamma analysis between synCT and CT calculated dose distributions. Nvol: number of PTVs.