2597
The Treatment Outcome of Magnetic Resonance guided High Intensity Focused Ultrasound Ablation of Uterine Fibroids through the Transverse and Longitudinal Scars1MR Therapy, Philips Healthcare, Seoul, Korea, Republic of, 2Department of Radiology, Pham Ngoc Thach University of Medicine, HCMC, Vietnam, Ho Chi Mihn City, Vietnam
Synopsis
This study investigates the technical treatment success and therapeutic efficacy of magnetic resonance guided high intensity of focused ultrasound (MR-HIFU) ablation of uterine fibroid patients with transverse and longitudinal scars. The results of the present study suggests that the scar patch could be used in MR-HIFU ablation of fibroid patients with transverse and longitudinal abdominal scars, which might no longer be regarded as an exclusion criterion.
INTRODUCTION
Magnetic resonance imaging (MRI) is of great importance in high intensity focused ultrasound (HIFU) treatments and used in not only patient selection but also treatment planning, temperature mapping and the prediction of the treatment outcome. Despite the clinical effectiveness of MR-HIFU for uterine fibroid treatment, the presence of both transverse and longitudinal scars in the ultrasound beam path is still considered to be one of the limiting factors1,2 as their presence might lead to undesired heat accumulation in the near field which could result in skin and subcutaneous tissue. To overcome this drawback, the safety assessment and technical feasibility of scar patch usage on fibroid patients with abdominal scars in MR-HIFU has been investigated3,4. However, there was no study to compare the treatment outcomes of MR-HIFU ablation between patients with transverse and longitudinal scar groups. Therefore, our aim in this study was to compare the immediate non perfused volume (NPV) ratio and the symptom severity score (SSS) improvement at follow-up between the two groups.
MATERIALS AND METHODS
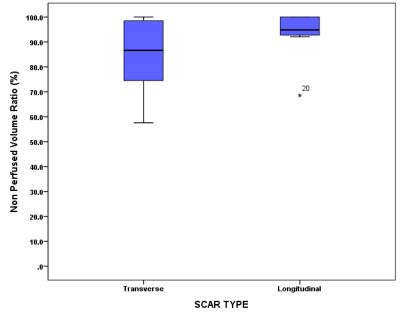
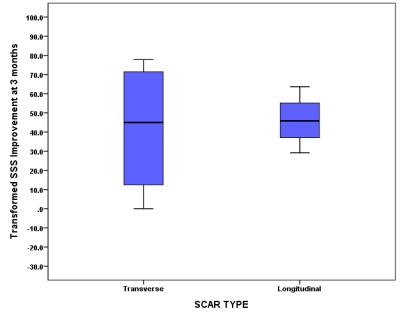
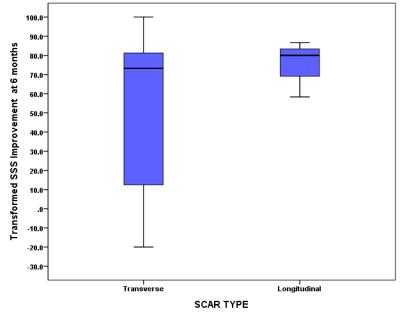
21 women (40.3±1.3 years with a range of 29–53 years) who underwent MR-HIFU ablation were divided into 2 groups: the transverse scar group (N=14) and longitudinal scars group (N=7). The immediate non perfused volume (NPV) ratio is defined as NPV measured by the immediate post HIFU contrast enhanced (CE)-T1-weighted (T1W) MR images, divided by the fibroid volume measured by the T2-weighted (T2W) images prior to the treatment. The questionnaire included the eight questions of SSS was measured at screening, 3 and 6 months follow-up5. The transformed SSS (tSSS) score was used in this study, yielding a 0 to 100 point scale with higher scores indicating worse symptoms. The Whisker boxplots were used to describe the relationship between the transverse and longitudinal scar groups for immediate post HIFU NPV ratio and tSSS improvement at follow-up.
RESULTS
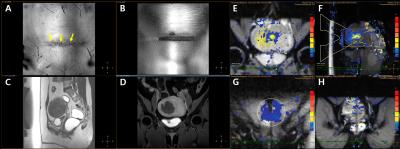
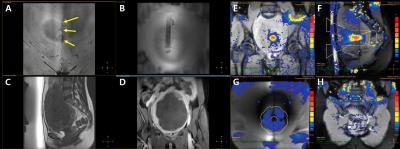
The diameter and volume of all fibroids were 62.2 mm ± 27.4 (26-150 mm) and 156.7 ml ± 164.7 (37.0-794.0 ml) for both groups, 58.9 mm ± 18.4 (32.0-95.0 mm) and 100.6 ml ± 59.0 (37.0-199.0 ml) for the transverse scar group and 68.8 mm ± 41.0 (26.0-150.0 mm) and 268.8 ml ± 246.7 (76-794 ml) for the longitudinal scar group, respectively. The transverse and longitudinal scar size in length was 135.0 mm ± 5.2.0 (26.0-232.0 mm) and 91.0 mm ± 39.0 (32.0–148.0 mm), respectively. The mean acoustic sonication power and treatment time from the first sonication to the last one were 139.3 W, 105.1 min for the transverse scar group and 137.1 W, 165.9 min for the longitudinal scar group, respectively. No significant difference in acoustic sonication power (P=0.864) and treatment time (P=0.072) were observed between the two groups. Figures 1 and 2 show an examples of transverse and longitudinal scars, scar patch, T2W MR images, MR temperature mapping and CE-T1W MR images, respectively. According to immediate follow-up CE-T1W MR images, the mean NPV ratio was 84.2% in the transverse scar group and 92.7% in the longitudinal scar group. Of the 21 patients, 3 and 6 months SSS follow-up data were available for 14 and 13 patients, respectively. With respect to symptom improvement between both scar groups, the tSSS improvement at 3 and 6 months follow-up were 42.2% and 53.9% for the transverse scar group and 46.1% and 75.0% for the longitudinal scar group, respectively. The Whisker Box plots show that no significant difference between both groups observed for immediate NPV ratio (P=0.204) and tSSS improvement at 3 and 6 months (P=0.805 at 3 months and P=0.433 at 6 months), respectively (Figures 3-5).
DISCUSSION
The results of the present study demonstrated that the immediate post HIFU NPV ratio and tSSS improvement at 3 and 6 months follow-up significantly decreased in each group (P<0.001) and no statistical significance was observed between the two groups. In conclusion, therefore, we suggest that that the scar patch could be used in the treatment of patients with transverse and longitudinal abdominal scars in MR-HIFU treatment procedure.
Acknowledgements
No acknowledgement found.References
1. Arleo EK, Khilnani NM, Ng A, Min RJ. Features influencing patient selection for fibroid treatment with magnetic resonance-guided focused ultrasound. J Vasc Interv Radiol 2007; 18:681-685.
2. Zaher S, Gedroyc WM, Regan L. Patient suitability for magnetic resonance guided focused ultrasound surgery of uterine fibroids. Eur J Obstet Gynecol 2009; 143:98-102.
3. Yoon SW, Seong SJ, Jung SG, et al. Mitigation of abdominal scars during MR-guided focused ultrasound treatment of uterine leiomyomas with the use of an energy-blocking scar patch. J Vasc Interv Radiol 2011; 22:1747-1750.
4. Zhu Y, Keserci B, Viitala A et al. Volumetric MR-guided high-intensity focused ultrasound ablation to treat uterine fibroids through the abdominal scars using scar patch: a case report. Journal of Therapeutic Ultrasound (2016) 4:20.
5. Spies JB, Coyne K, Guaou Guaou N et al. The UFS-QOL, a new disease-specific symptom and health-related quality of life questionnaire for leiomyomata. Obstet Gynecol. 2002; 99 (2):290-300.
Figures