2583
The value of 7T in the clinical evaluation of epileptic patients with tuberous sclerosis complex1State Key Laboratory of Brain and Cognitive Science, Beijing MRI Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, Beijing, People's Republic of China, 2University of Chinese Academy of Sciences, Beijing, People's Republic of China, 3Chinese PLA general hospital, Beijing, People's Republic of China, 4Beijing Tian Tan Hospital, Capital Medical University, Beijing, People's Republic of China
Synopsis
Tuberous sclerosis complex (TSC) is an autosomal dominant genetic disease. 90% of patients with TSC suffer from epilepsy and 50% of them become medicine intractable epilepsy. Epilepsy surgery is an important treatment. However, some focal epileptogenic lesions, essential for surgery, are not well identified by current routine imaging protocols at 3T. 7T MR imaging is assessed in this study to allow better characterization of lesion details and to detect abnormalities previously unseen on 3T MRI and scalp electroencephalogram (EEG). This is the first report of clinical application of 7T MRI for pediatric patients (older than 8 years) with TSC epilepsy.
Introduction
Tuberous sclerosis complex (TSC) is an autosomal dominant disorder resulted from mutations of TSC1 or TSC2 genes and is often associated with cortical tubers and intractable epilepsy for pediatric patients (1). Neurosurgical resection is often required to achieve seizure control. However, over 40% of epileptic patients with TSC do not show apparent focal abnormality with routine clinical sequences on conventional lower field MRI systems (2). In this work, 7T MRI with high spatial resolution and better tissue contrast was utilized to demonstrate improved visualization of TSC and to detect previously invisible TSC lesions within clinically reasonable time.Methods
Four patients (8-19 years old) were scanned at a 7T research system (Siemens, Erlangen, Germany) with volume transmit/32 channel receive head coil (Nova Medical). The study was approved by the Institutional Review Board of the Beijing MRI Center for Brain Research. Chloral hydrate was given per os for some young patients to decrease motion artifacts. 7T sequences including a high-resolution T1-weighted MPRAGE (0.6mm iso), WM-suppressed and GM/WM boundary–suppressed MPRAGE (0.7mm iso, TI=580ms/730ms) (3), 3D SPACE FLAIR (0.8mm iso) and T2-weighted TSE (0.3*0.3*2mm3) were performed. The techniques were compared with the corresponding routine sequences on conventional 3T MRI, including T1- and T2-weighted, and 2D FLAIR.Results
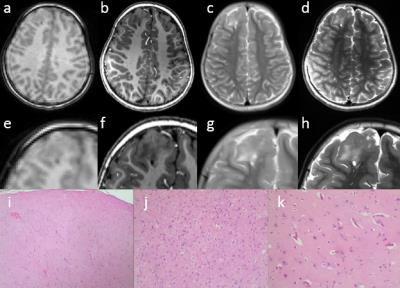
Case 1. The patient is an 8-year-old male diagnosed with TSC, who suffers from paroxysmal loss of consciousness. Electroencephalography (EEG) showed sharp and slow wave complex and sharp waves at the right anterior temporal lobe. Examination at 3T demonstrated multiple cortical tubers at the right frontal parietal and occipital lobes. 7T images revealed more clear margins of the frontal lesion (Fig.1) and showed abnormal hyperintense signal at the right hippocampal region (not shown here), which was not detected by 3T. Pathological diagnosis demonstrated disorder in cerebral cortex, proliferation of neuroglial cells and atrophy of neurons.
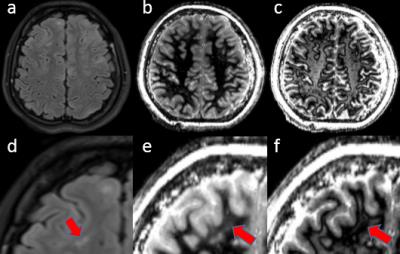
Case 2. The patient is a 19-year-old female diagnosed with TSC. The patient presented loss of consciousness and staring episodes after a high fever at 8 months. 3T showed multiple abnormal signals in cerebral parenchyma on 2D FLAIR images. The images were not well seen due to the larger slice thickness. The 3D high resolution SPACE FLAIR and WS-suppressed sequences at 7T revealed more details that were previously unperceived and detected new abnormality that was too subtle to be revealed at 3T (Fig.2).
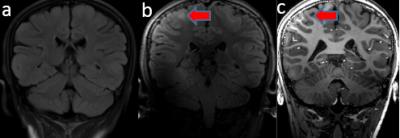
Case 3. The patient is an 11-year-old female diagnosed with TSC at age 2, when she suffered from episodes of distracted spirit and transient unconsciousness. Since then, she developed poor intelligence, hyperactivity, aprosexia and unsociableness. Multiple tubers were detected at 3T in the subcortical white matter and the borders of tubers were not clear. Examination at 7T improved the visualization of the tubers and their peripheral regions. Previously uncharacterized hyperintensive signals were detected at the frontal lobe (not shown here) and right parietal lobes (Fig.3).
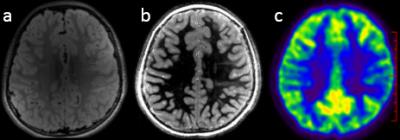
Case 4. The patient is an 8-year-old female diagnosed with TSC at 12 months. Since then, she presented with convulsions of limbs, eyes on the turn and uncoordinated body, which was resistant to numerous antiepileptic drugs. Mutation of TSC2 gene was detected. No obvious histological abnormality, except intracranial arachnoid cyst at the left frontal lobe, was detected by 3T. In contrast, the WM-suppressed images at 7T revealed previously undetected lesions, which had been validated by PET/CT results (Fig.4).
Discussions and Conclusions
To our best knowledge, 7T was assessed for the first time as a clinical approach to evaluate pediatric patients with TSC epilepsy. Although there were challenges including absent signals at the temporal lobe and deep brain regions caused by inhomogeneous B1 field, 7T provided prominent advantages in SNR, resolution, contrast, etc. In comparison with 3T, the improved spatial resolution and tissue contrast offered by 7T allowed more precise characterization of TSC lesions. 3D SPACE FLAIR and tissue signal suppression images based on the inversion recovery technique demonstrated more details around the tubers and detected previously unidentified subtle TSC abnormalities. Previous studies suggested that epileptogenicity of TSC was not originated from the tuber itself, but rather from the surrounding cortex (4,5). In this work, a hypothesis was proposed that the surrounding epileptogenic focus might be derived from the extension of tubers or subtle pathological abnormalities, which were not detected by conventional lower field MRI. This needed to be validated by further experiments.Acknowledgements
We thank Ms. Jing An (Siemens Shenzhen MR Ltd. China) for her technical assistance. This work was supported in part by Chinese MOST grants (2015CB351701, 2012CB825500), NSFC grant (91132302), and CAS grants (XDB02010001, XDB02050001).References
1. Crino PB, Nathanson KL, Henske EP. The tuberous sclerosis complex. N Engl J Med [Internet] 2006;355:1345–56.
2. Chalifoux JR, Perry N, Katz JS, Wiggins GC, Roth J, Miles D, Devinsky O, Weiner HL, Milla SS. The ability of high field strength 7-T magnetic resonance imaging to reveal previously uncharacterized brain lesions in patients with tuberous sclerosis complex. J. Neurosurg. Pediatr. [Internet] 2013;11:268–73.
3. Tourdias T, Saranathan M, Levesque IR, Su J, Rutt BK. Visualization of intra-thalamic nuclei with optimized white-matter-nulled MPRAGE at 7T. Neuroimage [Internet] 2014;84:534–545.
4. Kamimura T, Tohyama J, Oishi M, et al. Magnetoencephalography in patients with tuberous sclerosis and localization-related epilepsy. Epilepsia 2006;47:991–997.
5. Major P, Rakowski S, Simon M V., Cheng ML, Eskandar E, Baron J, Leeman BA, Frosch MP, Thiele EA. Are cortical tubers epileptogenic? Evidence from electrocorticography. Epilepsia 2009;50:147–154.
Figures