2514
High-Resolution MRI of Dental Ceramic Implants In Vivo1Department of Radiology, Medical Physics, Medical Center - University of Freiburg, Freiburg, Germany, 2Faculty of Medicine, University of Freiburg, Freiburg, Germany, 3Division of Oral and Maxillofacial Surgery, Medical Center - University of Freiburg, Freiburg, Germany, 4Department of Prosthodontics, Medical Center - University of Freiburg, Freiburg, Germany, 5Partner Site Freiburg, German Consortium for Cancer Research (DKTK), Heidelberg, Germany
Synopsis
The purpose of the study was to demonstrate the feasibility and evaluate the limitations of high-resolution MRI of ceramic implants in vivo. One healthy volunteer was subjected to high-resolution MRI before and after two zirconia dental implants were placed in the lower right jaw. Both implants were clearly depicted as signal voids, and no artifacts were observed using a turbo spin echo sequence. In conclusion, high-resolution in-vivo MRI of ceramic implants with an isotropic voxel size of (600 μm)3 is feasible within 5 minutes scan time.
Introduction
Dental implants are a routine treatment to replace missing teeth. The intervention is typically planned with 3D cone-beam computed tomography (CBCT), which, however, is not suited to control the outcome because of strong artefacts induced by the implant and the radiation exposure1,2. The use of metal free implants like zirconia enables the use of magnetic resonance imaging (MRI) to image oral implants postoperatively and has been demonstrated already ex vivo3. In this work, we seek to demonstrate the capability of MRI to image a zirconia implant in vivo for the first time.Methods
In this prospective study, written informed consent from a male volunteer (49 y) was obtained. The volunteer presented with a partially edentulous lower jaw and multiple composite, ceramic and metallic restorations of the teeth in the upper and lower jaw. Two zirconia (zirconium dioxide) implants with an endosseous diameter of 4.1 mm and a length of 8 mm (Fig. 1, ZERAMEX P6, Dentalpoint AG, Zurich, Switzerland) were placed in the lower right jaw (FDI positions 46 and 47). All MRI experiments were performed on a 3T clinical whole body scanner (MAGNETOM Prisma, Siemens Healthineers, Erlangen, Germany) and a 20-channel head coil (Siemens Healthineers, Erlangen, Germany). Within the coil, the head of the volunteer was fixed with cushions and the mandible was attached to the coil with medical tape to reduce motion. T1-weighted rapid acquisition with relaxation enhancement (RARE) imaging4 was performed prior and after implantation with the following parameters: TE/TR = 11/3750 ms, BW = 320 Hz/Px, matrix size = 240x320, FOV = 144x192 mm2, in plane resolution = 0.6x0.6 mm2, slice thickness = 0.6 mm, no slice gap. After automatic adjustments, 95 axial slices were acquired within a scan time of five minutes for visualization of the upper and lower jaw and identification of the dental implant region. MR images were acquired 21 days before and 7 days after intervention.
Results
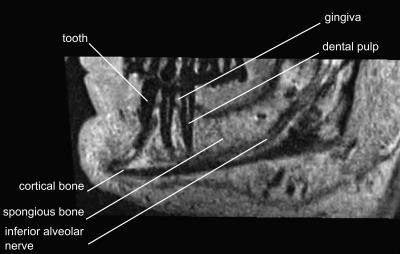
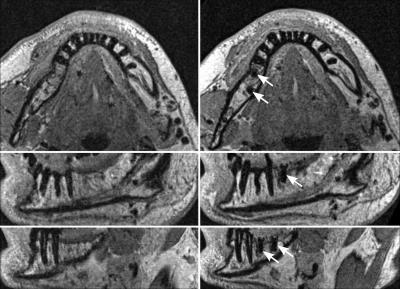
High-resolution MRI with an isotropic voxel size of (600 μm)3 acquired prior to the intervention clearly depicted the intraosseous course of the inferior alveolar nerve, soft tissues, and spongious bone (Fig. 2). No artifacts were exhibited after the intervention, both implants (as voids) and the surrounding tissue were fully depicted. The voids created by the implants corresponded to their physical size; within the given resolution, no distortions were apparent. Other metallic and composite restorations present in the mouth of the volunteer did not exhibit detrimental effects at the location of the implants (Fig. 3). The isotropic voxel size enabled the reconstruction of orthogonal planes at the same resolution, and arbitrary sliced with minimal loss.Discussion
High-resolution MRI of ceramic implants is feasible in clinically relevant scan times of approximately 5 min., enabling radiation-free monitoring of the implant and healing process. Isotropic resolution allows the reconstruction of arbitrary slices, which is important for accurate planning and monitoring. By choosing an appropriate contrast, we anticipate that this method will enable to identify pathologies such as inflammation or bone defects, which is not possible post-implantation with the current gold-standard, CBCT.Acknowledgements
We thank Dentalpoint AG, Zurich, Switzerland for providing both implants.References
1. Boas FE, Fleischmann D. CT artifacts: causes and reduction techniques. Imaging in Medicine 2012;4:229–240.
2. Barrett JF, Keat N. Artifacts in CT: Recognition and avoidance. RadioGraphics 2004;24:1679–1691.
3. Duttenhoefer F, Mertens ME, Vizkelety J, Gremse F, Stadelmann VA, Sauerbier S. Magnetic resonance imaging in zirconia-based dental implantology. Clin Oral Implants Res 2015;26:1195–1202.
4. Hennig J, Nauerth A, Friedburg H. RARE imaging: A fast imaging method for clinical MR. Magn Reson Med 1986;3:823–833.
Figures