2513
Assessing changes within the lumbosacral spinal cord in neurological disease: preliminary results of a pilot in vivo MRI study1UCL Institute of Neurology, Queen Square MS Centre, University College London, London, United Kingdom, 2UCL Institute of Neurology, Uro-Neurology, Department of Brain Repair & Rehabilitation, University College London, London, United Kingdom, 3Translational Imaging Group, Centre for Medical Image Computing, Department of Medical Physics and Biomedical Engineering, University College London, London, United Kingdom, 4UCL Institute of Neurology, Department of Molecular Neuroscience, University College London, London, United Kingdom
Synopsis
Magnetic resonance imaging (MRI)-derived tissue-specific measures of neuronal loss and demyelination were assessed at the lumbosacral level of the spinal cord (SC) in relation to neurological dysfunction. Acquisition of grey and white matter measures for the lumbosacral SC proved feasible, and were sensitive to detect tissue-specific changes in two neurological disorders commonly associated with lumbosacral cord involvement: Multiple system atrophy and Multiple sclerosis. This preliminary study demonstrates the utility of this cutting edge MRI acquisition method to detect pathological changes in the lumbosacral SC, and is a first step towards establishing new MRI biomarkers for these patient groups.
Purpose
Neurological diseases commonly affect the spinal cord (SC), resulting in significant impairment of mobility and other functions depending upon the level and location of lesion, and has a tremendous impact on health-related quality of life. Magnetic resonance imaging (MRI) has been used extensively to study the SC, and damage to the upper SC is associated with motor and sensory dysfunction in disorders such as Multiple sclerosis (MS)1. Moreover, specialised sequences such as magnetisation transfer imaging provide further insight into the pathophysiology of neurological diseases2,3. The lower SC plays a crucial role in the neurological control of lower limb and lower urinary tract (LUT) functions, however remains largely unexplored4. Recent studies in healthy volunteers have established new MRI acquisition and analysis protocols to identify the lumbosacral enlargement (LSE) and to obtain grey matter (GM) and white matter (WM) specific cross-sectional area (CSA) as well as magnetisation transfer ratio (MTR) measures2,5.
The objective of this study was to apply these protocols for the first time in neurological patients with clinical evidence for lower SC lesion. In MS, demyelinating lesions in this region may manifest with voiding difficulties and urinary retention. In an uncommon neurodegenerative disorder, Multiple system atrophy (MSA), progressive neuronal atrophy affects several regions of the central nervous system, particularly the lower SC, typically manifesting with early-onset LUT dysfunction and neurophysiological changes. The main aim of this pilot study was to test tissue-specific CSA and MTR measures obtained from the LSE in individuals with suspected neurodegenerative changes in the lumbosacral spinal cord, in relation to clinical symptom scores.
Methods
Eleven women with MS, Expanded Disability Status Scale (EDSS)<7 and reporting different degrees of LUT symptoms (e.g. without, mainly voiding, and/or storage problems), as well as 15 individuals with “probable MSA” (7 women) with clinical and neurophysiological features suggesting sacral SC dysfunction were included for this study. Corresponding healthy control (HC) groups were matched for age and gender. Group characteristics are summarized in Table 1. A cutting edge high-resolution 3T MRI acquisition protocol5 was used obtaining nineteen axial contiguous slices aligned perpendicular to the cord starting from the superior margin of the T11 vertebral body for individual detection of the lumbosacral enlargement (LSE) and to obtain mean cross-sectional area (CSA) of 3 slices spanning the LSE (LSE-CSA) and corresponding tissue-specific CSA (i.e. LSE-CSA-WM and LSE-CSA-GM) measures. A recently published MTR acquisition protocol2 was used providing corresponding MTR measures for the same SC segments (LSE-MTR, LSE-MTR-GM and LSE-MTR-WM). The Urinary Symptom Profile (USP) questionnaire was used to evaluate voiding and storage LUT symptoms. Neurological symptoms were assessed using the Unified Multiple System Atrophy Rating Scale (UMSARS) and EDSS in MSA and MS, respectively. For each patient group, tissue-specific CSA and MTR measures were compared with those of the respective HCs using multiple analyses of variance (MANOVA) with post-hoc tests. Exploratory correlations were calculated for MRI-derived measures with LUT and neurological symptom scores.Results
Table 2 summarizes mean MRI measures with corresponding group comparisons. Multivariate analyses of variance revealed a main effect for MSA across LSE-CSA-GM&WM assessments, F(2,25)=4.308, p=0.025, with a significant reduction in LSE-CSA-GM compared to HC, F(1,26)=8.960, p=0.006, when tested per tissue type. There were no significant effects (p>0.1) for MTR measures, gender or interactions. In MS, the MANOVA revealed a statistical trend, F(2,21)=2.917, p=0.76 across LSE-CSA-GM&WM assessments; with smaller LSE-CSA-GM in MS compared to HC (Table 2). Mean MTR measures seemed to be smaller but quite variable among individuals with MS and did not reach statistical significance.
In MSA, the degree of voiding symptoms was significantly (p<0.05) correlated with changes in CSA-GM, but with opposite changes in CSA-WM (increase in voiding difficulties à decrease in CSA-GM). In MS, however, voiding symptoms were related to changes in MTR assessments with smaller values relating to bigger voiding problems. Significant correlations were found for CSA-WM with decreasing values being related to larger storage symptom and EDSS scores.Discussion and Conclusion
For the first time, this recently established lumbosacral SC MRI assessment was shown to be feasible to use in neurological patients and was sensitive to detect tissue- and modality-specific abnormalities in individuals with MSA and MS, where lower SC involvement is clinically suspected. This study is an important initial step towards exploring new MRI biomarkers for the lumbosacral SC that may be useful to detect subtle symptom- and treatment-related changes in neurodegenerative conditions. A larger study, however, is required to confirm these findings and explore the utility of this MRI protocol across a larger spectrum of neurological disorders where the lower SC may be affected.Acknowledgements
ML received funding from the Swiss National Science Foundation (fellowship P2EZP3_148749 & P300PB_161087), joint research funding from UCL and the Neuroscience Center Zürich, and the UK Multiple Sclerosis Society. This work was also supported by the Medical Research Council, the UK Multiple Sclerosis Society (grant 892/08), the Brain Research Trust and by Capital Project number R&D03/10/RAG0449 from NIHR BRC UCLH/UCL. FP is funded by the National Institute for Health Research University College London Hospitals Biomedical Research Centre (NIHR BRC UCLH/UCL High Impact Initiative-BW.mn.BRC10269). CGWK receives funding from ISRT, Wings for Life and the Craig H. Neilsen Foundation for the INSPIRED study.References
1. Losseff NA, Webb SL, O'Riordan JI et al. Spinal cord atrophy and disability in multiple sclerosis. A new reproducible and sensitive MRI method with potential to monitor disease progression. Brain 1996;119:701-708.
2. Ugorji, CO, Samson RS, Liechti MD et al. Grey and White Matter Magnetisation Transfer Ratio Measurements in the Lumbosacral Enlargement: A Pilot In Vivo Study at 3T. PloS one 2015; 10:e0134495.
3. Yiannakas MC, Kakar P, Hoy LR et al. Feasibility of grey matter and white matter segmentation of the upper cervical cord in vivo: a pilot study with application to magnetisation transfer measurements. Neuroimage 2012;63:1054-9
4. Wheeler-Kingshott CA, Stroman PW, Schwab JM et al. The current state-of-the-art of spinal cord imaging: Applications. Neuroimage 2014;84:1082-93.
5. Yiannakas MC, Kakar P, Hoy LR et al. The Use of the Lumbosacral Enlargement as an Intrinsic Imaging Biomarker: Feasibility of Grey Matter and White Matter Cross-Sectional Area Measurements Using MRI at 3T. PLoS One 2014;9(8):e105544.
Figures
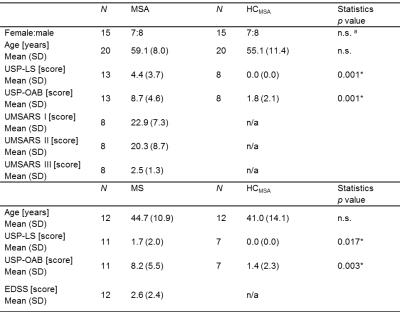
Table 1. N: sample size; Urinary Symptom Profile (USP) questionnaire providing voiding – i.e. low stream (USP-LS, score range: 0 to 9) and storage – i.e. overactive bladder (USP-OAB, score range: 0 to 21) symptoms; n.s.: Non-significant; N/A: Not applicable; Student’s t-tests and (a) Pearson’s chi-square tests with χ² values were used; * indicating statistical significance for p<0.05.
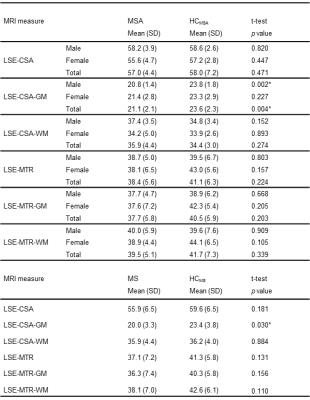
Table 2 Student’s t-tests were used; * indicating statistical significance for p<0.05. LSE: lumbosacral enlargement, CSA: Cross-sectional area, GM: Grey matter, WM: White matter, MTR: magnetisation transfer ratio.