2506
Motion-Free MR Imaging of Brachial Plexus using the PROPELLER technique combined with Low-Refocus Flip Angle FSE1Chiba Children's Hospital, Chiba, Japan, 2Tokyo Metropolitan University, Tokyo, Japan, 3Orthopaedic Surgery, Chiba Children's Hospital, Chiba, Japan, 4Eastern Chiba Medical Center, Chiba, Japan, 5Chiba Cancer Center, Chiba, Japan
Synopsis
The STIR Low-RFA PROPELLER method is a combination of STIR (Short-TI Inversion Recovery) suppressing fat signal homogenously and low refocus flip angle (Low-RFA) PROPELLER for flow signal reduction. Furthermore, the PROPELLER is able to reduce ghost generated by flow and motion, and to maintain high resolution by averaging of k-space. Consequently, the STIR Low-RFA PROPELLER method will be expected to produce clear brachial plexus imaging which is not affected by motion. In this study, we demonstrate that this new scheme (STIR Low-RFA PROPELLER) is superior to the conventional method (T2 weighted IDEAL) in the depiction of brachial plexus.
PURPOSE
Magnetic Resonance (MR) Imaging of the brachial plexus is useful for diagnosing the brachial plexus birth palsy.1 But, it is difficult for children to be quiet during MRI acquisition. Some authors have reported the efficacy of T2 weighted IDEAL water image to visualize the brachial plexus.2, 3 Although this method might be helpful for evaluating brachial plexus injury, it has several limitations such as blurring by long echo space, and long acquisition time. Furthermore, poor blood signal suppression disqualify the imaging. In this study, we propose a new scheme, that is motion-free MR Imaging of brachial plexus using the PROPELLER technique combined with low-refocus flip angle (Low-RFA) fast spin echo (FSE). We compared this new scheme (STIR Low-RFA PROPELLER) with conventional method (T2 weighted IDEAL) in the depiction of brachial plexus.METHODS
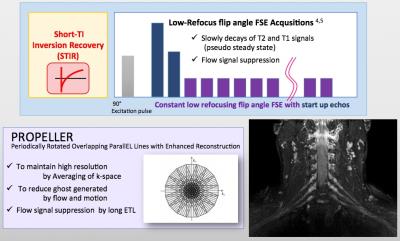
Theory: The STIR Low-RFA PROPELLER method is a combination of STIR (Short-TI Inversion Recovery) and Low-RFA PROPELLER. The former suppress fat signal homogenously, and the latter reduce noise from blood flow signal.4,5 Furthermore, the PROPELLER is able to reduce ghost and artifacts generated by flow and motion, and to maintain high resolution by averaging of k-space.6 (Fig.1) Consequently, the STIR Low-RFA PROPELLER method will be expected to acquire clear brachial plexus imaging.
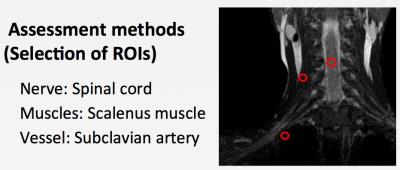
Experiments: Five normal volunteers were the subjects of this study (Male/Female = 4/1; 25-39 years, mean age 31.2years). All subjects were scanned by 1.5T (Tesla) MRI (Signa HDxt Ver.23, GE Healthcare) with HNS BrachPlx coil. The imaging parameters of Low-RFA PROPELLER sequence were as follows; coronal section, FOV = 280×280 mm, Matrix = 288×288, slice thickness/gap = 3/0 mm, slices = 22, acquisitions = 2, TR/TE = 3500/130 ms, ETL = 40, bandwidth (BW) = ±41.7 kHz, TI = 160, refocus FA = 45, over sampling factor = 1.4, NEX = 5 and total scan time of 5m12s. The imaging parameters of T2 weighted IDEAL sequence were as follows; fast recovery, coronal section, FOV = 280×280 mm, Matrix = 320×192, slice thickness / gap = 3/0 mm, slices = 22, acquisitions = 2, TR/TE = 2500/85 ms, ETL = 12, bandwidth (BW) = ±83.3kHz, NEX = 1 and total scan time of 4m56s. We evaluated 1) the effect of signal suppression from blood vessels, and 2) the signal intensity (SI) ratio between spinal cord and muscles or vessels. The former was examined by 3 trained radiologists with visual 5-point scale at subclavian artery, subclavian vein and carotid artery. The latter was calculated as follows: Nerve-to-muscle ratio = SI (nerve) / SI (muscle), Nerve-to-subclavian artery ratio = SI (nerve) / SI (artery). The Figure 2 shows the example of ROIs. This study was approved by our institutional review board, and written informed consent was obtained from all subjects.
RESULTS and DISCUSSIONS
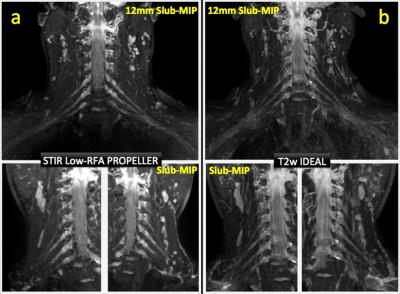
The Figure 3 shows that the Low-RFA PROPELLER was better for the flow signal suppression than the T2 weighted IDEAL. Figure 4 illustrates the differences of brachial plexus image. The Low-RFA PROPELLER could more effectively reduce signals from subclavian vessels than T2 weighted IDEAL. Moreover, it suppressed CSF flow signals, which could lead better to visualize nerve roots than T2 weighted IDEAL.
The T2 weighted IDEAL of brachial plexus was affected by the artifacts from flow, breathing and heartbeat. On the other hand, the Low-RFA PROPELLER was able to reduce these noises effectively. Since the PROPELLER method is a radial k-space sampling with parallel data lines rotating around the center of the k-space, which is able to correct spatial inconsistencies.6 And Low-RFA FSE acquisitions cause pseudo steady state (PSS), which produce robust flow signal suppression.7 Consequently, the STIR Low-RFA PROPELLER was able to produce clear brachial plexus imaging which is not affected by motion.
CONCLUSION
The Low-RFA PROPELLER can provide motion free imaging, which is able to reduce artifacts generated by flow, breathing and heartbeat. And it is more useful for flow signal suppression than T2 weighted IDEAL. Thus, the Low-RFA PROPELLER is an outstanding method to depict brachial plexus.Acknowledgements
No Acknowledgements found.References
1. Eismann EA, et al. Three-Dimensional Magnetic Resonance Imaging of Glenohumeral Dysplasia in Neonatal Brachial Plexus Palsy. J Bone Joint Surg Am. 2016 20; 98; 142-51.
2. Tagliafico A, et al. Usefulness of IDEAL T2 imaging for homogeneous fat suppression and reducing susceptibility artefacts in brachial plexus MRI at 3.0 T. Radiol Med. 2016 121: 45-53.
3. Omura N, et al. T2-weighted IDEAL fast spin echo imaging of the brachial plexus: comparison with STIR. Acta Radiol. 2015 56:1242-7.
4. Alsop DC. The sensitivity of low flip angle RARE imaging. Magn Reson Med 1997 37: 176-84.
5. Hennig J, Scheffler K. Easy improvement of signal-to-noise in RARE-sequences with low refocusing flip angles. Rapid acquisition with relaxation enhancement. Magn Reson Med. 2000 44: 983-5
6. Ohgiya Y, et al. MRI of the neck at 3 Tesla using the periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) (BLADE) sequence compared with T2-weighted fast spin-echo sequence. J Magn Reson Imaging. 2010 32; 1061-7.
7. Busse RF, et al. Effects of refocusing flip angle modulation and view ordering in 3D fast spin echo. Magn Reson Med. 2008 60: 640-9
Figures