2483
Functional connectivity depending on duration of parkinsonism before diagnosis of mild cognitive impairment in Parkinson Disease: focusing on the substantia innominata.1Department of Radiology, Ewha Womans University School of Medicine, Seoul, Korea, Republic of, 2Department of Radiology, Veterans Health Service Medical Center, 3Department of Neurology, Yonsei University College of Medicine, 4Department of Radiology, Yonsei University College of Medicine, 5Department of Radiology, Ewha Womans University School of Medicine
Synopsis
Degenerative change in the nucleus basalis of Meynert, a group of cholinergic neurons in the substantia innominata (SI) of the basal forebrain, begins in the early stages of Parkinson disease (PD) and is known to be significantly correlated with cognitive performance. We found decreased resting state functional connectivity (rsFC) in bilateral frontal areas using bilateral SI mask as a seed and significant correlation between decreased rsFC and shorter disease duration before mild cognitive impairment was diagnosed in patients with Parkinson’s disease. Therefore, our results support that cholinergic deficit plays an important role in the acceleration of cognitive decline and conversion to PD dementia.
INTRODUCTION
Degenerative change in the nucleus basalis of Meynert (NbM), a group of cholinergic neurons in the substantia innominata (SI) of the basal forebrain, begins in the early stages of Parkinson disease (PD) and is known to be significantly correlated with cognitive performance.1 We aimed to evaluate the different patterns of functional and structural changes in the SI of PD patients with mild cognitive impairment (PD-MCI) according to the duration of parkinsonism observed before mild cognitive impairment (MCI) was diagnosed using resting state functional magnetic resonance imaging (rsfMRI) and region of interest (ROI)-based volumetric analyses.
METHODS
Fifty-four patients with PD-MCI were classified into either the shorter (PD-MCI-SD, <1 year, n = 27) or longer (PD-MCI-LD, ≥1 year, n = 27) duration group according to duration of parkinsonism before MCI was diagnosed. Thirty-six age- and sex-matched drug-naïve PD patients with intact cognition (PD-IC) were included for comparison. Seed-based resting state functional connectivity (rsFC) analysis using the bilateral SI mask as a seed and ROI-based volumetric analysis were performed. Age, sex, years of education, age at onset of parkinsonism, and levodopa-equivalent dose were included as covariates.RESULTS
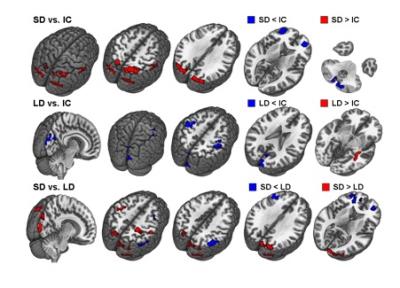
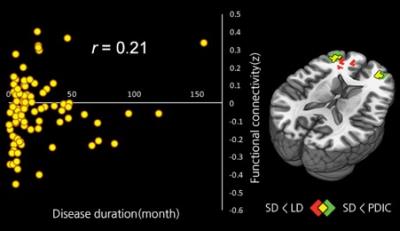
Compared to the PD-IC group, the collapsed PD-MCI group (PD-MCI-SD and PD-MCI-LD; n=54) showed decreased rsFC in the left frontal area, while increased rsFC was observed in the bilateral parietal areas (Figure 1). Compared to the PD-IC group, the PD-MCI-SD group exhibited decreased rsFC in the bilateral frontal areas, while increased rsFC was observed in the bilateral parietal areas. The PD-MCI-LD group exhibited decreased rsFC in the bilateral primary motor sensory areas and cuneus, and increased rsFC in the right temporal area compared to the PD-IC group. In a direct comparison between the PD-MCI-SD and PD-MCI-LD groups, the PD-MCI-SD group showed decreased rsFC in both the frontal and right parietal areas. On the other hand, the PD-MCI-LD group showed decreased functional connectivity in the bilateral primary motor sensory areas and both occipital areas (Figure 2). Moreover, Spearman’s correlation analysis showed significant associations between shorter disease duration with decreased rsFC in both frontal areas (rho= 0.212, P = 0.047; Figure 3). The mean SI volumes for the three groups were as follows: PD-IC, 0.999±0.157ml; PD-MCI-LD, 0.981±0.174ml; and PD-MCI-SD, 0.957±0.186ml, respectively. The PD-MCI-SD group showed the lowest value; however, there were no significant differences across the groups statistically (P=0.650).DISCUSSION
Decreased rsFC in the left frontal area and increased rsFC in the bilateral parietal areas was observed in collapsed PD-MCI compared to PD-IC when the bilateral SI mask was used as a seed, suggesting these areas are relevant to cognitive dysfunction in PD patients. The PD-MCI-SD group showed rsFC alteration in broader cognitive dysfunction related areas compared to PD-IC as well as the PD-MCI-LD groups without significant structural changes in SI. Among these areas, the decreased rsFC between the bilateral SI seed and both frontal areas had significant correlation with shorter disease duration in PD patients, supporting previous results2 which suggested that cholinergic deficit played an important role in the acceleration of cognitive decline and conversion to PD dementia.CONCLUSION
Our results suggest that decreased rsFC between the SI and bilateral frontal areas might be a sensitive and noninvasive neuroimaging biomarker that reflects cortical cholinergic denervation in the NbM which also predicts rapid cognitive decline. This altered rsFC can become a future therapeutic target for novel treatment modalities (e.g., transcranial direct current stimulation or transcranial magnetic stimulation). Furthermore, this could be used to identify suitable PD patients for targeted cholinergic drug treatment and to monitor treatment effect. To enable these clinical applications, a subject-level diagnostic and prognostic model should be first established.Acknowledgements
No acknowledgement found.References
1. Braak, H., et al., Staging of brain pathology related to sporadic Parkinson's disease. Neurobiol Aging, 2003. 24(2): p. 197-211.
2. Kehagia, A.A., R.A. Barker, and T.W. Robbins, Cognitive impairment in Parkinson's disease: the dual syndrome hypothesis. Neurodegener Dis, 2013. 11(2): p. 79-92.
Figures