2467
Evaluating the clinical outcomes of patients with occlusion of the middle cerebral artery using susceptibility-weighted imaging1Tianjin First Central Hospital, Tianjin, People's Republic of China, 2Radiology Department, Tianjin First Central Hospital, Tianjin, People's Republic of China
Synopsis
In this study, we used the susceptibility-weighted imaging and mapping technique (SWIM) to investigate the effect of vessel susceptibility when evaluating the severity of cerebral infarction to develop an early prognosis of patients with middle cerebral artery thrombosis. By analyzing thrombus length, thrombus susceptibility, clot burden score, and the Admission and Discharge National Institute of Health Stroke Scale (NIHSS) scores between groups divided by the presence or absence of a deep medullary vein (DMVs) and between groups divided by the presence or absence of an asymmetrically prominent cortical vein (APCVs), we found that patients with a DMVs or APCVs were not affected by the burden factors of a thrombus. Compared to an APCV, a DMV suggests the presence of a larger cerebral infarction and is associated with an increased discharged NIHSS score, indicating a poor short-term prognosis.
Introduction
Deep medullary veins (DMVs) and asymmetrically prominent cortical veins (APCVs) have been observed in ischemic stroke1, 2. Although the relationship between DMVs/APCVs and stroke prognosis have been explored in previous studies, controversy persists about the impact of DMVs and APCVs on prognosis. In this study, we explored the relationship between DMVs, APCVs, middle cerebral artery (MCA) thrombosis, the size of cerebral infarction, and Admission and Discharge National Institute of Health Stroke Scale (NIHSS) scores in patients with MCA occlusion using the susceptibility-weighted imaging and mapping technique (SWIM).Methods
A total of 73 patients were retrospectively included in our study. The inclusion criteria were: 1) the middle cerebral artery territory showed hyperintensity on diffusion-weighted imaging (DWI) and hypointensity on apparent diffusion coefficient (ADC) images; 2) the patient had a unilateral MCA occlusion confirmed by Time-of-Flight MR Angiography (TOF-MRA) and corresponding thrombosis confirmed by susceptibility-weighted imaging (SWI); 3) the clinical information and imaging information were complete. The exclusion criteria were: 1) the patient had MR contraindications; 2) the patient had bilateral MCA occlusion; 3) the patient had other diseases, including cerebrovascular malformations, tumor, brain trauma, neuropsychiatric disorder, hemorrhage, or previously undergone neurosurgery. The patients were divided into a DMVs group (16 patients), a non-DMVs group (57 patients), an APCVs group (41 patients), and a non-APCVs group (32 patients) based on the imaging evidence of DMVs/APCVs (Fig. 1). MRI data were collected on a MAGNETOM Trio Tim 3T MR scanner (Siemens, Erlangen, Germany), including a routine head scan plus a SWI scan. The parameters of SWI were: TR/TE=27/20ms; field of view=230×200mm2; receiver bandwidth=120 Hz/pixel; flip angle=15°; number of slices=56; acquisition time=179 sec; voxel size=0.5×0.5×2.0mm³. SWIM was reconstructed using both phase and magnitude data, and using SMART (Susceptibility Mapping and Phase Artifacts Removal Toolbox, Detroit, Michigan, USA) software. The length and susceptibility of the MCA thrombus were measured using SPIN (Signal Processing in Nuclear Magnetic Resonance, Detroit, Michigan, USA) software (Fig. 1), and the thrombus length in SWIM images was kept the same as that in SWI images. The thrombus segment (single or multiple segments), length, susceptibility, and clot burden score (CBS) were recorded. The DWI-Alberta Stroke Program Early CT score (DWI-ASPECTS) was measured to estimate the size of cerebral infarction. The NIHSS scores were also assessed. The differences in thrombus length, thrombus susceptibility, CBS, DWI-ASPECTS, and NIHSS scores in the groups with/without DMVs or in the groups with/without APCVs were explored using two independent sample t-tests and the Mann-Whitney U test. The difference in the presence of APCVs between the group with/without DMVs was explored using a chi-square test.Results
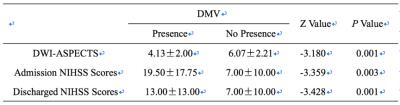
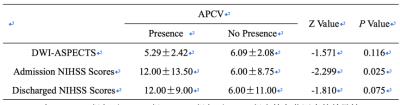
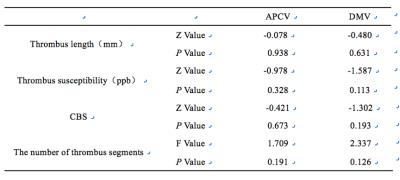
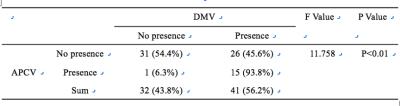
The DWI-ASPECTS scores of the different groups are shown in Table 1. The admission NIHSS scores in the APCVs group were significantly higher than those in the non-APCVs group (P=0.025). There was no statistically significant difference in DWI-ASPECTS and discharged NIHSS scores between APCVs group and non-APCVs group (P>0.05) (Table 2). There was no significant difference in the thrombosis length, thrombus susceptibility, CBS scores, and the number of thrombus segments between the DMVs group and the non-DMVs group and between the APCVs group and the non-APCVs group (P>0.05) (Table 3). There was a statistically significant difference in the presence of APCVs between DMVs group and non-DMVs group (P=0.001) (Table 4). 93.8% of patients in the DMVs group had the presence of APCVs.Discussions
We found that the DWI-ASPECTS score of the non-DMVs group was significantly higher than that of the DMVs group. We also found that the admission NIHSS scores and the discharged NIHSS scores of the DMVs group were significantly higher than those of the non-DMVs group, indicating that the presence of DMVs suggested more severe cerebral infarction. The reason may be that severe cerebral infarction can cause total cerebral hemisphere ischemia, decreased cerebral blood velocity, and increased deoxyhemoglobin in the DMVs4, all of which can increase the clarity of the DMVs. In our study, we found that admission NIHSS scores in the APCVs group were significantly higher than those in the non-APCVs group, suggesting that the presence of APCVs also correlated with more severe cerebral infarction. The mechanism underlying the presence of APCVs may be that ischemic brain tissue results in decreased cerebral blood velocity and increased deoxyhemoglobin in the cortical veins1, 5. The presence of a DMV or APCV was not affected by thrombus-related burden factors, such as the thrombus length, thrombus susceptibility, CBS scores, or the number of thrombosis segments.Conclusions
The presence of DMVs indicates a larger size of cerebral infarction and increased discharged NIHSS score, suggesting poor short-term prognosis.Acknowledgements
The contribution of each author to the work was listed as followed: Shuang Xia (S.X.): substantial contributions to conception and design; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; Chao Chai (C.C.): substantial contributions to conception and design, acquisition of data, or statistical analysis and interpretation of data; Qingyuan Yang(Q.Y.Y.): contributions to conception and design; acquisition of data, or analysis and interpretation of data; Sile Hu(S.L.H.): acquisition of data, or analysis and interpretation of data; Tianyi Qian (T.Y.Q.): analysis and interpretation of data; E Mark Haacke (E.M.H.): substantial contributions to conception and design; analysis and interpretation of data; revising it critically for important intellectual content; Wen Shen (W.S.): substantial contributions to conception and design.References
[1] Xia S, Utriainen D, Tang J, et al. Decreased oxygen saturation in asymmetrically prominent cortical veins in patients with cerebral ischemic stroke [J]. Magn Reson Imaging, 2014, 32(10): 1272-1276.
[2] Han X, Ouyang L, Zhang C, Ma H, Qin J. Relationship between deep medullary veins in susceptibility-weighted imaging and ipsilateral cerebrovascular reactivity of middle cerebral artery in patients with ischemic stroke. Exp Ther Med. 2016 Jun;11(6):2217-2220.
[3] Haacke EM, Tang J, Neelavalli J, Cheng YC. Susceptibility mapping as a means to visualize veins and quantify oxygen saturation. J Magn Reson Imaging. 2010 Sep;32(3):663-76.
[4] Mucke J, Möhlenbruch M, Kickingereder P, Kieslich PJ, Bäumer P, Gumbinger C, Purrucker J, Mundiyanapurath S, Schlemmer HP, Bendszus M, Radbruch A. Asymmetry of deep medullary veins on susceptibility weighted MRI in patients with acute MCA stroke is associated with poor outcome. PLoS One. 2015 Apr 7;10(4):e0120801.
[5] Sun W, Liu W, Zhang Z, et al. Asymmetrical cortical vessel sign on susceptibility-weighted imaging: a novel imaging marker for early neurological deterioration and unfavorable prognosis [J]. Eur J Neurol, 2014, 21(11): 1411-1418.
Figures
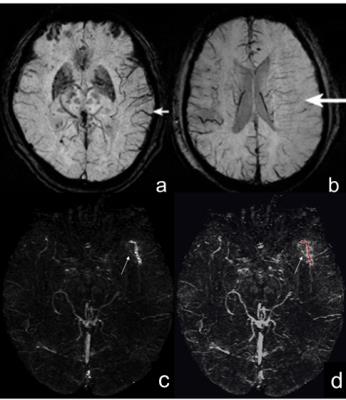
Fig. 1 Imaging of APCVs, DMVs and thrombus length measurement in SWIM images.
a. The left asymmetrically prominent cortical veins (APCVs) are clearly visible in the SWI minimum intensity projection image.(short arrow) b. The deep medullary veins (DMVs) perpendicular to the long axis of the ventricle within the left cerebral hemisphere are visible in the SWI minimum intensity projection image.(long arrow) c. The thrombus showed a linear-like pattern of high signal intensity in the SWIM images (arrow). d. the red line represented the measurement of thrombus length.