2459
The diagnostic utility of high-resolution 3D T1-weighted SPACE imaging in patients with intracranial vertebrobasilar dissecting aneurysms.BINBIN SUI1, PEIYI GAO1, YAN LIN1, YISEN ZHANG2, TIANYI QIAN3, and XINJIAN YANG2
1RADIOLOGY, BEIJING TIANTAN HOSPITAL, CAPITAL MEDICAL UNIVERSITY, BEIJING NEUROSURGERY INSTITUTE, BEIJING, People's Republic of China, 2NEUROINTERVENTION, BEIJING TIANTAN HOSPITAL, CAPITAL MEDICAL UNIVERSITY, BEIJING NEUROSURGERY INSTITUTE, BEIJING, People's Republic of China, 3MR Collaborations NE Asia, Siemens Healthcare, BEIJING, People's Republic of China
Synopsis
The purpose of this study is to investigate the application value of a 3D high-resolution fat-saturated (FS) T1 SPACE sequence for the diagnosis of intracranial vertebrobasilar dissecting aneurysm (VBDA). With sub-millimetric and nearly isotropic acquisition, the 3D T1-SPACE sequence demonstrated good sensitivity and specificity for the detection of the imaging features associated with VBDAs using a large coverage area and a thin slice thickness.
Introduction
East Asian populations demonstrate a higher incidence of VBDAs than other populations. High-resolution magnetic resonance imaging (HR-MRI) could be a useful imaging technique for diagnosing intracranial VBDAs noninvasively. However, conventional two-dimensional black-blood sequences are limited by their long acquisition time. This study aims to demonstrate the value of a 3D fat-saturated (FS) T1-weighted SPACE (T1-SPACE) sequence with application-optimized contrast in detecting intracranial VBDAs within a shorter imaging timeframe.Methods
We retrospectively reviewed 34 patients (27 male, 7 female, with ages ranging from 18 to 82 years, with a median age of 52 years) with unruptured intracranial VBDAs that were confirmed by digital subtraction angiography (DSA). MR images were performed on a MAGNETOM Trio Tim 3T MR scanner (Siemens Healthcare, Erlangen, Germany) with a 32-channel head coil. HR-MRI included T2W-TSE, dark-blood T1W-TSE, MPRAGE, and 3D T1-SPACE sequences. Eighteen patients underwent a post-contrast T1-SPACE scan as well. The 3D T1-SPACE sequence was acquired in the oblique coronal plane and fat saturation with the following parameters: TR/TE=800/22ms, voxel size= 0.7 x 0.7 x 0.7mm3, FOV=240x160mm2, matrix=320x240. Multi-planar reconstructions (MPR) were performed to visualize the dissection from different planes of the T1-SPACE images. Two neuroradiologists, each with at least 5 years of experience in vascular neuroimaging, independently assessed the HR-MR images. They were blinded to the imaging type. They evaluated whether the following signs of dissection were visible on the 2D and 3D images: intramural hematoma (IMH), double lumen, dissection flap, and outer-diameter enlargement.Results
Thirty-five VBDAs were found in 34 patients with two lesions found in one patient. Eighteen were located at the right vertebral artery (RVA), 9 at the left vertebral artery (LVA), 7 at the basilar artery (BA), and one involved both the BA and LVA. Most VBDAs presented an outer-diameter artery enlargement in different degrees on the axial HR-MR images (33/35, 94.3%). The maximum outer diameter of all the VBDAs was 6-39mm with an average value of 15.9±8.2mm. IMHs, were best detected with MPRAGE, and found in 60.0% (21/35) of cases. Using MPRAGE, double lumens were observed in 85.7% (30/35) of cases, and dissection flaps were detected in 77.1% (27/35) of cases. With the contrast-enhanced T1-SPACE images, dissection flaps were found in 16 of 18 cases (87.5%). Overall sensitivity and specificity for the T1-SPACE sequence were 0.914 and 0.971, respectively; the sensitivity and specificity of T1-TSE were 0.829 and 0.942,respectively. Additionally, T1-SPACE could detect all IMHs. With MPR reconstruction of the thin-slice sequences, dissection flaps were found in 71.4% (25/35) cases, which was higher than on the 2D T2WI (20/35) images. Despite a shorter acquisition time (4 min 17 s for 3D T1 SPACE versus 5 min 35s for 2D T1-TSE dark-blood sequence), the 3D T1 SPACE sequence compared to the 2D T1-TSE sequence had a larger scanning area that could cover the whole intracranial segment of both vertebral arteries and the basilar artery.Discussion
The wall structures and the classical features of VBDAs can be well visualized by HR-MRI, which provided important compensatory information for DSA. T1-SPACEoffered several advantages for the detection of the features of VBDAs compared with 2D axial imaging. 3D acquisition with sub-millimetric and isotropic resolution (0.7x0.7x0.7mm3 in this study), and multi-planar reconstruction allowed for observation from different angles with good image quality. Its optimized contrast improved the detection of dissection aneurysms and dissection flaps as well. Another advantage of the SPACE sequence was a large field of view in the z-axis. For intracranial imaging, the coronal acquisition can cover the entire intracranial segment of the vertebral arteries and the basilar artery with a shorter acquisition time. Previous studies have used 3D SPACE imaging to image carotid dissections. In our study we have demonstrated that imaging features of VBDAs including IMH, double lumens, dissection flaps, and outer-diameter enlargement can be detected in most patients by T1-SPACE imaging in this study.Conclusions
The high-resolution T1-SPACE sequence demonstrated good visualization of features of VBDAs with a large coverage area and a thin slice thickness. Multiplanar reconstruction of 3D source images improved the detection of dissection flaps.Acknowledgements
This work is supported by by National Natural Science Foundation of China (81301193), NSFC-NIH joint program (81361120402) and Beijing Natural Science Foundation(7162056)References
[1] Debette S, Compter A, Labeyrie M A, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection[J]. Lancet Neurol,2015,14(6):640-654.
Figures
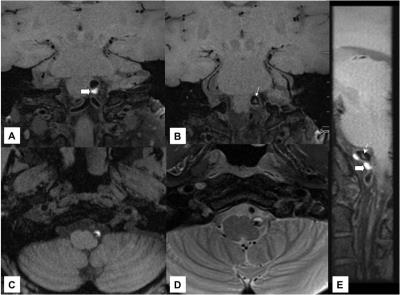
Fig 1. A
51-year-old female patient with a dissection at the LVA.(A, B)3D SPACE T1
images show the IMH (thick white arrow) and the dissection flap (small black
arrow) in the lumen. (C) MP-RAGE sequence detected the IMH displaying a high
signal intensity at the LVA wall. (D) T2WI show a high signal intensity of the
vessel wall and a low signal intensity of the lumen. (E) The oblique sagittal
reformation of 3D SPACE T1 image clearly display the IMH (thick white arrow)
and the dissection flap (small white arrow).
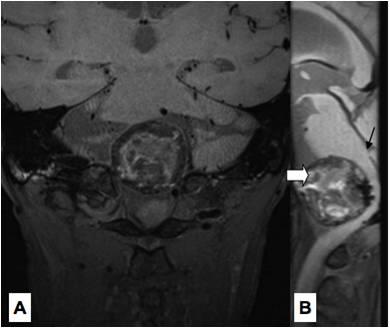
Fig 2. A
68-year-old male patient with a large dissection aneurysm at the LVA. The outer
diameter was clearly enlarged. (A, B) A heterogenous signal intensity was found
in the lesion, which indicated IMH and thrombosis of the dissection aneurysm. The
large coverage of the 3D SPACE T1 imaging allowed for better visualization of
the lesion and the adjacent structures.