2458
Arterial Spin Labeling Evaluation of Severity of Hypoperfusion in Symptomatic Intracranial Atherosclerotic StenosisJinhao Lyu1,2, Ning Ma3, Bing Wu4, Xiaoxiao Ma1, Lin Ma1, Zhongrong Miao3, and Xin Lou1
1Radiology, Chinese PLA General Hospital, Beijing, People's Republic of China, 2Jincheng General Hospital, People's Republic of China, 3Beijing Tiantan Hospital, Capital Medical University, Beijing, People's Republic of China, 4GE healthcare China, Beijing, People's Republic of China
Synopsis
Multiple post labeling delay arterial spin labeling provide dynamic perfusion information in patients with intracranial artery atherosclerostic stenosis, and is of useful to study collatera circulation. In this study, two PLD ASL was used to evaluate the severity of hypoperfusion in patients with unilateral middle cerebral artery (MCA) stenosis and we found that the severity of hypoperfusion assessed by two PLD ASL was significantly correlated with collateral circulation and associated with recurrent ischemic stroke in these patients.
Introduction
Assessing collateral circulation in patients with intracranial atherosclerotic stenosis conveys great clinical significance as it is effective to compensate cerebral perfusion1. Conventional approach for such assessment has been relying the perfusion assessed by dynamic susceptibility contrast imaging2. On the other hand, arterial spin labeling is a non-invasive approach in assessing the status of cerebral blood perfusion. Although past studies have reported the use of ASL in assessing hemodynamic impairments in patients with intracranial athrosclerotic stenosis(ICAS), only a single post labeling delay time was used and only information related to final perfusion level is available. We hypothesize that the use of multiple PLD ASL and studying of the difference in perfusion level with varying PLDs may better reveal the dynamic perfusion information that is related to the slow blood flow of collateral circulation, and hence may be used as a viable biomarker for predicting the stroke recurrence. In this study, two PLD ASL was used to evaluate the severity of hypoperfusion and its relationship with collateral circulation and recurrent ischemic stroke in patients with unilateral middle cerebral artery (MCA) stenosis.Method
This retrospective study included consecutive patients diagnosed with severe 70% to 99% athrosclerotic stenosis in unilateral middle cerebral artery by digital subtraction angiography (DSA) and MR angiography. All the patients underwent ASL imaging with two PLDs of 1.5s and 2.5s on a 3.0T whole body scanner (MR750, GE, USA). Cerebral blood perfusion (CBF) maps were on vendor supplied work station (AW4.6, GE, USA). The volumes of hypoperfusion were identified by an experienced radiologist on CBF maps corresponding to both PLDs. Severity of hypoperfusion was defined as hypoperfusion ratio(HR) that was derived as [hypoperfusion volume at 2.5s / hypoperfusion volume at 1.5s X 100%]. For patients where DSA results were available, the level of collateral was graded according to ASITN/SIR grading system on a 4-point scale. Statistical correlation between HR and the collateral circulation grades was performed. Patients were then followed up after 6 months to record whether a transit ischemic attack (TIA) or stroke recurred. The correlation between the HR and recurrence was also performed. Baseline characteristics including risk factors, time from sympton onset to MRI, national institutes of health stroke scale(NIHSS) were compared between patients with recurrent stroke and without using student’s t test or non-parametric test and X2 test or Fisher’s exact test when appropriate.Results
A total of 37 patients (47.1±11.8 years; 25 men) were included in this study, and DSA was available for 17 patents. DSA and multiple-PLD ASL images of patients with collateral grade 1-3 are shown in Fig.1-3, varying levels of hypoperfusion may be seen with increasing collateral grades. The correlation of HR and the collateral grades is shown in Fig 4. It is seen that HR was significantly correlated with collateral grades (r=-0.40, p=0.0493). In 6 months, 7 patients were confirmed to have a recurrent TIA or Stroke in the same territory. In the table of Fig 5, it is seen that the HR and NIHSS were significantly higher in the recurrence group, whereas other baseline characteristics had no significantly different between two groups.Conclusion
In this study, two PLD ASL was an useful approach in assessing the extent of collateral circulation in patients with ICAS. Hemodynamic impairments indexed by severity of hypoperfusion as revealed by HR and NIHSS may be effective indicators for stroke recurrence. Further study is warranted.Acknowledgements
No acknowledgement found.References
1. Liebeskind DS. Collateral circulation. Stroke. 2003;34:2279-2284
2. Bang OY, Goyal M, Liebeskind DS. Collateral circulation in ischemic stroke. Stroke. 2015;46:3302-3309
Figures
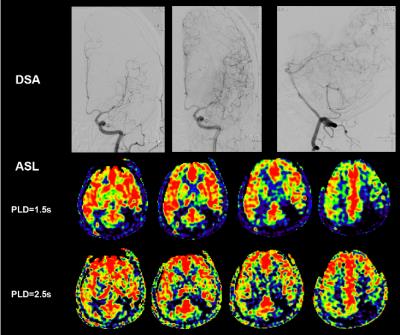
Fig 1 A 52-year-old male patient with left M2 segment severe stenosis shows inadequate collateral within MCA territory on DSA and is assessed as ASITN/SIR grade 1. Slow and only a few inflow can be seen on CBF map from 1.5s to 2.5s. Hypoperfusion is still observed on 2.5s CBF map. Hypoperfusion ratio is measured as 62.6%. The patient had experienced a recurrent stroke in the subsequent 6 months.
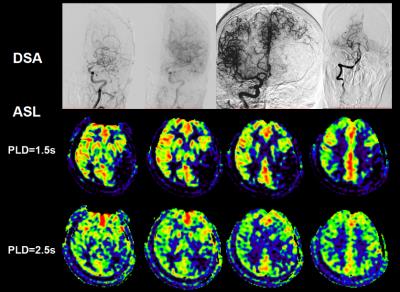
Fig 2 A 52-year-old female patient with left M1 segment severe stenosis shows leptomeningeal collateral from ACA to MCA and is assessed as ASITN/SIR grade 2. Slow inflow can be seen on CBF map from 1.5s and 2.5s though hypoperfusion region is still present on 2.5s CBF map. Hypoperfusion ratio is measured as 29.5%. ACA: anterior cerebral artery.
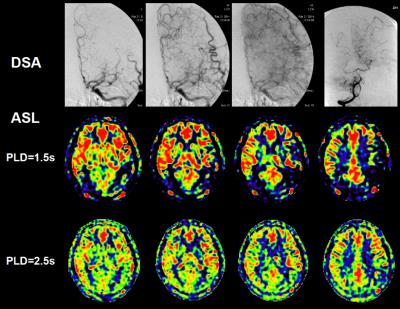
Fig 3A 51-year-old male patient with left M1 segment severe stenosis shows slow and complete collateral compensation within MCA territory on DSA and is assess as ASITN/SIR grade 3. Obvious slow inflow can be seen from 1.5s and 2.5s, and therefore only a very small hypoperfusion volume can be observed on 2.5s CBF. Hypoperfusion ratio is measured as 10%.
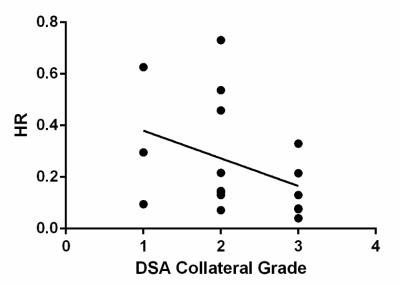
Fig 4 Scattered plots shows the relationship of collateral grade and HR in patients with an available conventional angiography. The line represents linear regression.
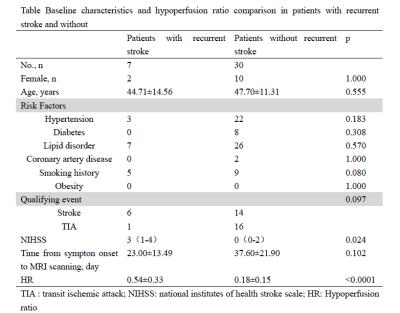
Fig 5 Table