2456
Comparison of two different measurement methods in evaluating basilar atherosclerotic plaque using high resolution MRI 3 T1Radiology, Changhai Hospital of Shanghai, Shanghai, People's Republic of China
Synopsis
Evaluation of morphologic characterization of BA plaque (such as plaque area, stenosis rate and percent plaque burden) is significant and may guide treatment decisions in clinical setting. In this study, we employed the maximal lumen narrowing sites as the referenced sites to calculate morphologic parameters. This study aims to compare the Referenced and Self-referenced measurement method methods in assessing basilar atherosclerotic plaque employing dark blood HRMRI at 3 Tesla. The present study found Self-referenced method is more convenient and even better for evaluating BA plaque.
Purpose
An atherosclerotic plaque at the basilar artery (BA) is frequently observed in patients with ischemic strokes and TIA of the posterior cerebral circulation [1]. The state-of-art MRI technology, especially at 3T field strength, offers significant improvement in signal-to-noise, vessel wall to lumen contrast-to-noise ratio and image quality compared to imaging at 1.5T [2]. High-Resolution magnetic resonance imaging (HRMRI) has emerged in recent years as an effective tool for assessing plaque in the intracranial arteries. Evaluation of morphologic characterization of BA plaque (such as plaque area (PA), stenosis rate (SR) and percent plaque burden (PPB)) is significant and may guide treatment decisions in clinical setting. Previous studies used the nearest plaque-free or minimally diseased segments proximal and distal to the maximal lumen narrowing (MLN) sites as referenced sites to calculate morphologic parameters (here referred to Referenced measurement method) [3,4]. In this study, we employed the MLN sites as the referenced sites to calculate morphologic parameters (here referred to Self-referenced measurement method). We hypothesized that Self-referenced measurement method is better than Referenced measurement method in evaluating plaque morphologic characterization. To the best of our knowledge, no such study has reported at present. Therefore, the goal of this study is to compare the above two methods in assessing basilar atherosclerotic plaque employing dark blood HRMRI at 3 Tesla.Materials and methods
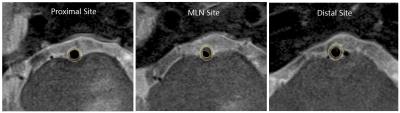
Subjects Thirty-seven patients (28 males and 9 females, 47-79 years old, mean age = 62 years) with >20% stenosis as identified by conventional MRA were recruited. The present study was approved by the local institutional review board and written informed consent was obtained from each patient. MRI protocol Cross-sectional imaging was performed on a 3T MRI system (Skyra, Siemens medical solution, Germany) using a standard 20-channel phased-array head/neck coil. 3D time of flight (TOF) images were used for HRMRI image positioning and obtained with TR/TE = 21/3.4 ms, FOV = 180×200 mm2, matrix = 330×384, thickness = 0.7 mm, and average = 1; parameters for 2D T2 weighted turbo spin echo (T2W TSE) were TR/TE = 2890/46 ms, FOV = 100×100 mm2, matrix = 256×256, thickness =2 mm, ETL = 20, and averages = 2. Image analysis The images were reviewed by an experienced observer, who was blinded to the clinical information of each patient. Outer wall areas, inner wall areas and lumen areas of proximal sites, MLN sites and distal sites were traced manually by the observer (Figure 1). The calculation of PA, SR and PPB using Referenced measurement method were referred to a previous study [4]. For Self-referenced measurement method, PA= inner wall area - lumen area, SR = 1- plaque area/ inner wall area, PPB = plaque area/outer wall area. To test the intraobserver variability, the observer measured BA plaque twice during two different time points that were separated by a 2-week interval to avoid any recall bias. Statistical analysis Significant difference between Self-referenced and Referenced measurement methods for repeated measurements of PA, SR and PPB were assessed by using two-tailed paired t-test. Agreement between repeated measurements was quantified through intraclass correlation coefficient (ICC), coefficient of variation (CV) and Bland-Altman plots.Results
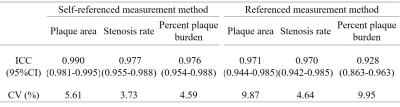
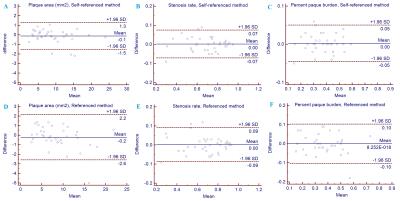
There were no significant difference in PA, SR and PPB between the two measurement methods (all P values >0.05). The ICCs and CVs of two measurement methods were summarized in table 1. Both methods have an excellent agreement in evaluation of BA plaque, but the CVs of Self-referenced is lower than Referenced measurement method. Moreover, Bland-Altman plots also showed that Self-referenced method has a narrower interval and less variability than Referenced measurement method (Figure 2).Discussion and Conclusion
This study found that an excellent reproducibility for quantifying PA, SR and PPB of basilar atherosclerotic plaque using both methods and had no significant difference between two methods, which is important for quantifying morphologic parameters of plaque and further studies. However, Self-referenced method is more convenient and better for evaluating BA plaque. Self-referenced method may serve as a promising method for evaluating basilar atherosclerotic plaque.Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant Number 31470910) and the Shanghai Shenkang Porject of Shanghai, China (Grant Number SHDC12013110).References
1. Mamatha H, D'Souza AS, Pallavi, Suhani S. Human cadaveric study of the morphology of the basilar artery. Singapore Med J. 2012;53(11):760-763.
2. Vidal A, Bureau Y, Wade T, Spence JD, Rutt BK, Fenster A, Parraga G. Scan-rescan and intra-observer variability of magnetic resonance imaging of carotid atherosclerosis at 1.5 T and 3.0 T. Phys Med Biol. 2008;53(23):6821-6835.
3. Feng C, Xu Y, Bai X, Hua T, Li Q, Tang GY, Chen YJ, Liu XY, Huang J. Basilar artery atherosclerosis and hypertensive small vessel disease in isolated pontine infarctions a study based on high-resolution MRI. Eur Neurol. 2013;70(1-2):16-21.
4. Zhu XJ, Du B, Lou X, Hui FK, Ma L, Zheng BW, Jin M, Wang CX, Jiang WJ. Morphologic Characteristics of Atherosclerotic Middle Cerebral Arteries on 3T High-Resolution MRI. AJNR Am J Neuroradiol. 2013;34(9):1717-1722.
Figures