2454
Imaging findings in patients with pulsatile tinnitus using black-blood MRI: a retrospective study1Center for Biomedical Imaging Research, Department of Biomedical Engineering, School of Medicine, Tsinghua University, Beijing, People's Republic of China, 2Neurosurgery department of the general hospital of PLA, Beijing, People's Republic of China, 3Xuanwu Hospital, Capital Medical University, Beijing, People's Republic of China, 4Department of Otolaryngology Head and Neck Surgery, Beijing Tongren Hospital, Capital Medical University, Beijing, People's Republic of China, 5Department of Radiology, University of Washington, Seattle, United States
Synopsis
In this study, we used black-blood (BB) MRI to investigate and classify venous wall abnormalities among PT patients, and found that venous vessel wall anomalies played an important role in PT mechanism. Arachnoidal granulations overgrowth, congenital stenosis, double-lumen, arterio-venous fistula, mastoiditis and malformation were observed in this retrospective study. In conclusion, BB imaging has the potential to provide more pathological information and guide surgical treatment of PT, which is of great clinical value.
INTRODUCTION
Pulsatile tinnitus (PT) accounts for 4% of all tinnitus patients[1]. Various causes, especially abnormalities of transverse- and sigmoid-sinus are reported in previous studies[2,3]. Among those studies, CT/CTA and MRA/V were mainly used for characterizing PT patients, in which vessel and temporal bone were frequently studied. But the role of venous vessel wall and surrounding tissues in PT mechanism is not well discussed. Black-blood (BB) MRI is an emerging tool for characterization of vessel wall conditions and can be used for cerebral venous thrombosis imaging[4]. In this study, we aim to investigate and classify venous wall abnormalities using black-blood (BB) MRI among venous PT patients.METHODS
Subjects:
31 consecutive patients (4 male and 27 female, age = 20~58 yrs) with clinical diagnosed PT, who underwent MR scan at our institution between July 2015 and October 2016, were included in this study. All subjects were approved by the local ethics committee and written informed consent were obtained.
MR protocol and image analysis:
All MR scans were performed on a 3T MRI scanner (Philips Achieva, Best, Netherlands). For evaluation of transverse- and sigmoid-sinus, T1-weighted, DANTE-VISTA[5,6] sequence was used in our study. Imaging parameters were: TR/TE = 800/19 ms, FOV = 200 x 180 x 50 mm3, acquired voxel size = 0.7 x 0.7 x 0.7 mm3. MR venography scan was also used in this study. Imaging parameters were: TR/TE = 22/4.6 ms, flip angle = 10°, FOV = 220 x 160 x 144 mm3, acquired voxel size = 0.9 x 1.2 x 1.6 mm3, VENC = 15cm/s. Demographic data including gender and age, along with side of PT, were collected for patients. Drainage dominance, defined by a 20% difference in the size of transverse sinuses, was investigated using MR venography, Readers interpreted BB images to identify venous stenosis, defined as a 30% reduction in caliber of the vessel, and other abnormalities. All BB images were exported to a Philips workstation where curved multi-planar reconstructions were created. Statistical analysis was performed using MedCalc (MedCalc Software, Mariakerke, Belgium).
RESULTS
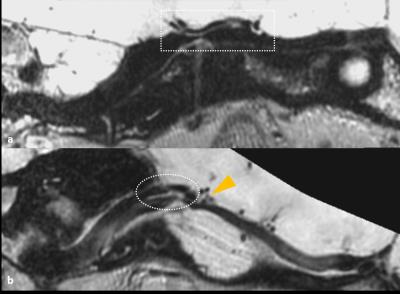
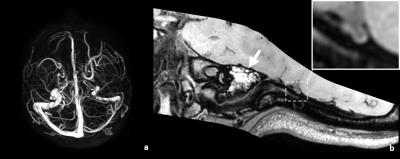
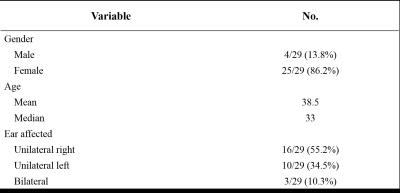
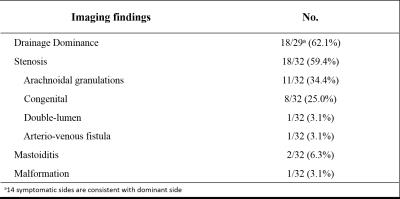
Of 31 patients, 29 patients and 32 veins on symptomatic side can be clearly seen and were included in this study. Two cases were excluded because of the poor image quality caused by motion. Table 1 shows the demographics of this population. Imaging findings are summarized in Table 2. Drainage dominance (18/29, 62.1%) and stenosis (19/32, 62.5%) are two main characteristics of PT patients. Overall, 14 symptomatic sides are consistent with dominant side. We also found that, arachnoidal granulations (11/32, 34.4%) and congenital stenosis (8/32, 25.0%) are two causes of stenosis (Fig.1 shows examples). Other anomalies (mastoiditis (Fig.3), 2/32, 6.3%; double lumen (Fig.2b), 1/32, 3.1%; arterio-venous fistula (Fig.2a), 1/32, 3.1% and malformation, 1/32, 3.1%) were also observed in this study.DISCUSSION
In this study, we successfully imaged the venous anomalies using BB imaging techniques among patients with PT. According to demographic and clinical data, our study found a high PT prevalence of female to male (25 female vs. 4 male), which is consistent with previous studies[2]. MR Venography showed a high prevalence in drainage dominance (18/29, 62.1%) of which most (14/18) were in the symptom side, further indicating that drainage dominance might be one marker of PT. Conventional techniques, such as DSA, CTA/V, or MRA/V, can only find the stenosis, while BB MRI images can identify the reason of stenosis. In this study, with BB images, we found that arachnoidal granulations overgrowth was frequently observed, which should be an important cause of stenosis in transverse-sinus. In addition, we found that anatomical anomalies can cause stenosis, such as arterio-venous fistula and double-lumen. Stenosis are often associated with an increase of blood velocity, resulting in turbulence flow in sigmoid-sinus, which is widely considered as the source of bruit[3]. However, our study did not found obvious stenosis in 40% patients, indicating the bruit causing venous flow are not only caused by stenosis. Since mechanism of PT is complicated, there can be several possible causes occurring at the same time, as shown in Fig.2b and Fig.3. More importantly, differentiate those sources of tinnitus using BB imaging technique is essential for treatment selection. For example, knowing the double lumen condition could help the surgeon a lot in stenting.CONCLUSION
In conclusion, venous vessel wall anomalies played an important role in PT mechanism. Our study showed that BB imaging has the potential to provide more pathological information and guide surgical treatment of PT, which is of great clinical value.Acknowledgements
No acknowledgement found.References
[1] Lockwood AH, et al. N Engl J Med 347(12):904–10.
[2] Stephen S, et al. Otolaryngol Head Neck Surg 150(5): 841–6.
[3] Zhao P, et al. Eur Radiol (2016) 26:9–14.
[4] Yang Q, et al. Stroke, In Press.
[5] Wang J, et al. Magn Reson Med (2016) 75:831-38.
[6] Viessmann O, et al. Magn Reson Med, In Press.
Figures