2450
The role of serotonin in cerebral blood flow and oxygen metabolism in migraine1Radiology, University of Californai San Diego, La Jolla, CA, United States, 2Neurology, Scripps Clinic, La Jolla, CA, United States
Synopsis
We examined the CBF and CMRO2 changes that accompany menstrual migraine, and evaluated the response to sumatriptan to determine the role of serotonin in migraine pathophysiology. Migraine is accompanied by a decline in global CBF and CMRO2 that appears to be serotonin-mediated. There is also a decline in stimulus-dependent CBF to a visual stimulus, that appears to also involve serotonin, but acts differently from the global responses. A decline in visual stimulus-dependent CMRO2 is not serotonin mediated, and appears to follow the normal variation in stimulus-dependent CMRO2 response that changes with normal menstrual cycle.
Introduction
Migraine is a highly prevalent chronic condition characterized by a hyper-responsive nervous system that predisposes to recurrent episodes of severe headache and autonomic disturbance. The etiology remains unclear, and a vascular vs. neuronal debate continues. We use calibrated BOLD fMRI and ASL / TRUST to evaluate changes in cerebral blood flow and metabolism during migraine episodes, and determine the role of serotonin based on their response to treatment with a serotonin receptor agonist, sumatriptan.Methods
5 female patients with ICHD-II diagnosis of menstrual migraine were recruited (patients were otherwise healthy with no additional cerebrovascular or neurological pathology). CBF and CMRO2 data were acquired at 3 time points: (1) Baseline (during symptom-free luteal phase of menstrual cycle), (2) Migraine (during headache - typically day 1 of cycle), (3) Post treatment on same day, 2 hrs following 6mg sc aerosol injection of sumatriptan (Sumavel DosePro). To control for variations in CBF and CMRO2 with menstrual cycle, 5 healthy female controls also underwent the same MR measurements at the same time points and also received the sumatriptan injection. For simultaneous acquisition of CBF and BOLD time series, we used a dual echo spiral PICORE QUIPSS II (FOV=256mm, TR=2500ms, TI1=700ms, TI2=1750ms, TE1=3ms, TE2=30ms, 6x 7mm slices, 64x64 matrix) 1. R2* relaxation was calculated from the 2 echoes, allowing direct comparison of BOLD signals across the 3 separate measurements sessions 1 2. Subjects viewed an 8Hz alternating checkerboard to evaluate the visual fMRI response during migraine and following sumatriptan. Visual cortex was defined from a separate functional localizer scan to the same 8Hz checkerboard. Resting CBF / BOLD was acquired during 3.5 minutes of steady state. A separate ASL/BOLD time series during a 5% CO2 calibration stimulus was collected and used to calculate the CMRO2 response in the visual cortex using the Davis BOLD signal model 3. High-resolution anatomical MRI 2 was also collected for registering data between sessions. Venous SvO2 in sagittal sinus is measured with TRUST MRI (T2-Relaxation-Under-Spin-Tagging) 2 4. From this, we determined oxygen extraction fraction (OEF) and global CMRO2Results
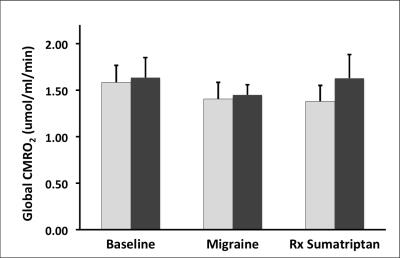
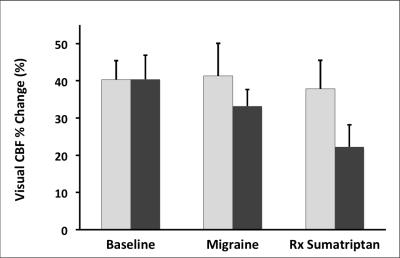
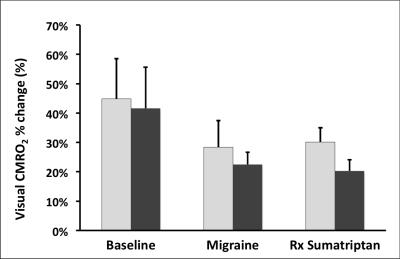
Whole brain CBF in control subjects showed no significant effect of menstrual cycle, and remained constant across the 3 measurements, and in particular there was no change in global blood flow following the sumatriptan injection (figure 1). In migraine patients, there was a 15% decline in mean blood flow during the migraine headache (P < 0.05 one tailed), which was reversed by sumatriptan. Global CMRO2 showed a similar trend with 11% decline in CMRO2, which responded to sumatriptan (figure 2). Control subjects also showed no significant difference in their CBF response in visual cortex to the checkerboard stimulus across the 3 measurements. However, patients showed a 20% decrease in CBF response during their migraine headache. This was not reversed by sumatriptan (and actually declined further) (figure 3). Control subjects showed a decline in the CMRO2 response in visual cortex to the checkerboard stimulus at menstrual cycle day 1. A similar trend was also seen in migraine patients, with no recovery following sumatriptan.Discussion
Migraine headache is accompanied by a decline in global CBF and global CMRO2. This appears to act via serotonin, and is reversed by sumatriptan treatment. In visual cortex, the normal CBF response to a standard visual stimulus is also seen to decline with migraine headache. However, the further decline in CBF with sumatriptan may indicate a different serotonin mechanism than the global CBF changes. There is also a decline in the CMRO2 response to a visual stimulus during menstrual migraine, but this seems to follow the normal change in stimulus-dependent CMRO2 response during the normal menstrual cycle, and is not serotin dependent.Acknowledgements
Supported by NIH R21 NS091709References
1. Perthen JE, Lansing AE, Liau J, Liu TT, Buxton RB. Caffeine-induced uncoupling of cerebral blood flow and oxygen metabolism: a calibrated BOLD fMRI study. Neuroimage 2008;40(1):237-47.
2. Smith ZM, Krizay E, Guo J, Shin DD, Scadeng M, Dubowitz DJ. Sustained high-altitude hypoxia increases cerebral oxygen metabolism. J Appl Physiol 2013;114(6):832.
3. Davis TL, Kwong KK, Weisskoff RM, Rosen BR. Calibrated functional MRI: mapping the dynamics of oxidative metabolism. Proc. Natl. Acad. Sci. USA 1998;95:1834-39.
4. Lu H, Ge Y. Quantitative evaluation of oxygenation in venous vessels using T2-Relaxation-Under-Spin-Tagging MRI. Magn Reson Med 2008;60(2):357-63.
Figures