2432
Increased Anisotropy as Possible Compensatory Plasticity of Ventral Thalamic Nuclei to Gait Disturbance in Patients with Idiopathic Normal Pressure Hydrocephalus1Department of Radiology, School of Medicine, College of Medicine, Taipei Medical University, Taipei, Taiwan, 2Department of Medical Imaging, Taipei Medical University Hospital, Taipei, Taiwan, 3Translational Imaging Research Center, College of Medicine, Taipei Medical University, Taipei, Taiwan, 41Department of Biomedical Imaging and Radiological Sciences, National Yang-Ming University, Taipei, Taiwan, 5Department of Radiology, Tri-Service General Hospital, Taipei, Taiwan, 6Graduate Institute of Biomedical Electrics and Bioinformatics, National Taiwan University, Taipei, Taiwan, 7School of Biomedical Engineering, College of Biomedical Engineering, Taipei Medical University, Taipei, Taiwan, 8Department of Medical Imaging and Radiological Sciences, Kaohsiung Medical University, Kaohsiung, Taiwan
Synopsis
This study allows improved localization of sensorimotor-related thalamic nuclei providing non-invasive evaluation of the microstructural changes of thalamus after iNPH, which may have a potential to contribute to early diagnosis and better prognosis prediction in the patients.
Introduction
Idiopathic normal pressure hydrocephalus (iNPH) is characterized clinically by gait disturbance, urinary incontinence and cognitive decline [1]. While the exact cause of the iNPH remains unclear, abnormal absorption of CSF with a consequent accumulation of CSF in the ventricular space has been observed. Gait disturbance is typically the most prominent clinical feature in the early stage of iNPH, possibly resulting from abnormal interactions of motor and sensory activities in the brain. Although it could be improved after a diversion of CSF via a ventriculoperitoneal shunt, the procedure is sort of invasive and risky, implying the importance of patient selection criteria for shunt surgery and an urgent demand for further understanding of the neurophysiological mechanism. On the other hand, the ventral nuclei, such as VA, VL, and VPL, of the thalamus play an important role in the modulation of sensorimotor circuit [2]. Recent advances in diffusion tensor imaging (DTI) allow specific tracking of fibers passing through the nuclei, and the quantification of anisotropy in terms of metrics such as the fractional anisotropy (FA) offers insight into the microstructural alternations. Therefore, this study aims to examine the diffusion tensor parametric behavior of the sensorimotor-related nuclei in response to gait disturbance in normal pressure hydrocephalus.Method
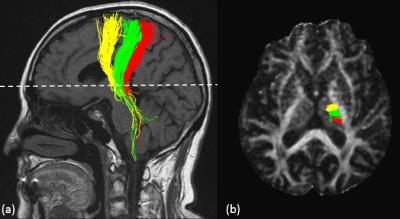
15 NPH patients and 15 normal controls were enrolled in this study. NPH patients were diagnosed according to Japanese guidelines for management of idiopathic NPH [3]. After the conventional MR examinations on a 1.5T scanner (GE, Signa HDx, USA), a phase-contrast gradient-echo sequence (TR=45, TE=12 ms, FA=20o) with a maximum encoding velocity of 20 cm/sec was used to assess the alteration of dynamic CSF flow. Moreover, DTI was performed using single-shot echo-planar imaging technique with parameters as follows: TR=10000 ms; TE=85.3 ms; flip angle=90o; b values=0, 1000 seconds/mm2; diffusion directions=15; FOV=240; matrix size=128×128 (zero-filled to 256×256); section thickness=4 mm; section gap=0 mm; and NEX=2. After data acquisition, fiber-tracking was performed using MRtrix software package (Brain Research Institute, Melbourne, Australia, http://www.brain.org.au/software/) based on probabilistic streamlines method. As to the segmentation of the motor-related nuclei, the tract-based scheme proposed by Yamada et al. [4] was performed using two inclusion ROIs for propagation of fibers: one was placed at the ventral thalamus, and the other was placed at the motor-related cortices including the supplementary motor area, primary motor cortex, and primary somatosensory cortex, respectively. The FA values inside the three motor-related thalamic nuclei (VA, VL, VPL) and the CSF flow velocity of iNPH patients and controls were calculated for further comparisons.Results
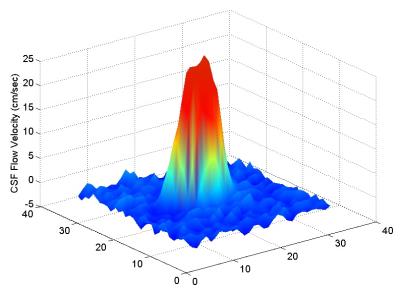
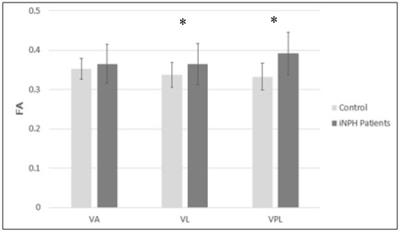
First, quantifications of the CSF flow in asymptomatic subjects and iNPH patients were performed on the aqueduct region. Increased mean peak flow velocity was found in the iNPH group as compared to that of controls (< 10 cm/s) (Fig.1). Fig. 2(a) showed the results of fiber-tracking on the sensorimotor-related brain structures, in which the fiber tracts projected to the supplementary motor area (yellow), primary motor cortex (green), and primary somatosensory cortex (red), were segmented, respectively. The cross section covering the axial FA map with the biggest thalamic area was chosen for identifying the regions of VA, VL as well as VPL (Fig. 2(b)). In addition, mean FA values in the sensorimotor-related nuclei (VA, VL and VPL) of the two groups were presented in Fig 3. Although there were no significant differences of FA values in VA between two groups, the FA values in VL and VPL of the iNPH patients significantly increased as compared to that of controls (P < 0.05).Discussion
To our best knowledge, this is the first study to explore the relationship between alterations of CSF flow velocity as well as the microstructural changes of sensorimotor-related thalamic nuclei in patients with iNPH. The processing of motor function involving several brain structures and sensorimotor circuits, can be quite sophisticated, implying the possibility of neural reorganization and compensatory plasticity of the circuits after motor impairment. Previous report has demonstrated the importance of somatosensory processing and its effects on motor control [5]. In our preliminary result, significant increase of FA in VL and VPL was observed in iNPH patient at acute stage, suggestive of the important role in modulation and coordination of the sensorimotor function during acute period. This is also in concert with the concept of early rehabilitation intervention for motor improvement in iNPH patient. In conclusion, tract-based tracking method allows improved localization of sensorimotor-related thalamic nuclei providing non-invasive evaluation of the microstructural changes of thalamus after iNPH, which may have a potential to contribute to early diagnosis and better prognosis prediction in the patients.Acknowledgements
This study was supported by the Ministry of Science and Technology, Taipei, Taiwan (MOST 105-2221-E-038-006)References
1. Williams MA, Relkin NR, et al. Diagnosis and management of idiopathic normal-pressure hydrocephalus. Neurol Clin Pract. 2013; 3(5):375-385
2. Planetta PJ, Schulze ET, Geary EK, et al. Thalamic projection fiber integrity in de novo Parkinson disease. AJNR 2013; 34(1):74-9
3. Ishilawa M, Hashimoto M, Kuwana N, et al. Guidelines for management of idiopathic normal pressure hydrocephalus. Neurol Med Chir (Tokyo) 2008; 48 Suppl: S1-23
4. Yamada K, Akazawa K, Yuen S, et al. MR imaging of ventral thalamic nuclei. AJNR 2010; 31(4):732-5
5. Patel N, Jankovic J, Hallett M. Sensory aspects of movement disorders. Lancet Neurol. 2014; 13(1):100-12.
Figures