2427
Impact of the topology of brain microbleeds on the structural brain network1Department of Diagnostic Radiology, The University of Hong Kong, HKSAR, People's Republic of China, 2The State Key Laboratory of Brain and Cognitive Sciences, The University of Hong Kong, HKSAR, People's Republic of China, 3Department of Medicine, The University of Hong Kong, HKSAR, People's Republic of China, 4Li Ka Shing Faculty of Medicine, The University of Hong Kong, HKSAR, People's Republic of China
Synopsis
We aim to investigate the effect of the topology of brain microbleeds (BMBs), lobar (n = 32) versus deep/infratentorial (n = 31), on structural brain network in patients with TIA or first-time stroke. Our results demonstrated that the efficiency of the local and global networks of both BMB cohorts were lower compared to controls (n = 31), and that only the load of the patients with lobar BMBs was strongly associated with decrease in the efficiency of local and global networks independent of vascular risk factors. These findings suggested that lobar and deep BMBs likely have distinct pathophysiological underpinnings.
Purpose
Cerebral small vessel disease is a leading cause of cognitive decline and functional loss in the elderly 1, a plausible culprit of which has recently been suggested as the brain microbleeds (BMBs) 2–4. Importantly, the location of which could be a potential marker of the underlying vascular pathology 5, and that those located in the lobar region would lead to worse cognitive function 4. In this study, we therefore aim to investigate the effect of the topology of BMBs on the structural brain network.
Materials and Methods
Participants n = 94 patients with TIA or first acute stroke were recruited. n = 63 had BMBs, and n = 31 did not and were considered as controls and matched with the former by age, gender and stroke diagnosis.
BMBs identification The location and number of BMBs were assessed by two observers on SWI images. Patients were dichotomized based on BMB location 3 – Lobar (n = 32): strictly in cortical gray matter (GM) or subcortical/periventricular white matter (WM); deep (n = 31): in lobar and deep (basal ganglia, thalamus, corpus callosum, internal, external and extreme capsules) or infratentorial (brainstem and cerebellum) region.
Experiment and data analysis DWIs were acquired using single-shot EPI, b-value of 1000 s/mm2 along 32 directions and 3T Achieva TX (Philips Healthcare). 90 regions were segmented using the AAL atlas and FSL. Tractography and network metrics were obtained using the Diffusion Toolkit (trackvis.org/dtk/) and Brain Connectivity Toolbox6, respectively. One-way ANOVA followed by Bonferroni post-hoc analysis was performed. Partial correlations between network metrics and BMB count for the two BMB cohorts were performed. All analyses were controlled for age, sex, hypertension, presence of TIA/infarct/lacunar infarct, brain and infarct volumes.
Results
Compared to controls, the global network of both BMB cohorts had increased characteristic path length (p < 0.001) and lower global efficiency (lobar / deep: p = 0.01 / 0.02). The lobar cohort had lower nodal efficiency in the anterior cingulate (p = 0.018), superior temporal (p = 0.022), middle temporal (p = 0.006), and superior frontal (p = 0.021) gyri (Figure 1). The deep cohort had lower nodal efficiency in the anterior cingulate (p < 0.001), superior frontal (p < 0.01), superior temporal (p = 0.016) gyri, supplementary motor area (p = 0.001) and insular (p = 0.017) as well as the pallidum (p < 0.001) and putamen (p = 0.013) (Figure 1). There was no significant difference between the structural brain network of the two BMB cohorts.
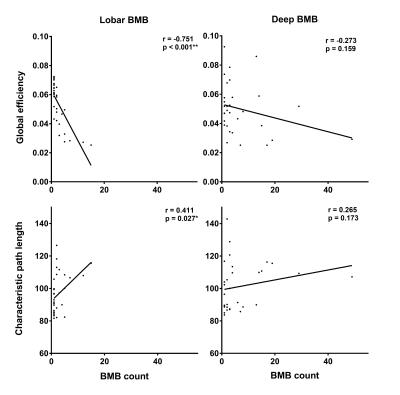
Only the characteristic path length (r = 0.411, p = 0.027) and global efficiency (r = -0.751, p < 0.001) of the lobar cohort were significantly correlated with BMB count (Figure 2). The nodal efficiency of the anterior cingulate (r = -0.571, p = 0.001), superior temporal (r = -0.510, p = 0.005) and superior frontal (r = -0.683, p < 0.001) gyri of the lobar cohort were also correlated with BMB count (Figure 3). After controlling for hypertension, no significant correlation was found between nodal efficiency and BMB count for the deep cohort (Figure 3).
Discussion
The major findings of this study are that, amid decrease in the efficiency of the local network, which was more widespread for the deep cohort, and global network as a result of BMBs, the effect of which on the lobar cohort is more gradual, whilst that together with hypertension, or hypertension alone, on the deep cohort likely has an all-or-nothing effect. Another noteworthy finding is that all changes in the local network of the lobar cohort were localized in the cerebral cortex, such as the superior frontal 7, anterior cingulate 8 and superior temporal 9 gyri, which are responsible for higher cognitive functions, whilst those of the deep cohort were widespread. These results likely indicated that the pathophysiological underpinnings of the two BMB cohorts are very different. It was indeed suggested that BMBs located in lobar regions could be marker for cerebral amyloid angiopathy, whilst those in the deep or infratentorial regions for hypertensive arteriolosclerosis 3. The former were also found to be associated with longitudinal cognitive decline but not the latter 4.
Conclusion
Our findings suggested that lobar and deep BMBs affect structural brain networks very differently. That increase in the lobar BMB load is strongly associated with decrease in the efficiency of local and global networks, suggesting that distinct pathophysiological underpinnings are likely.Acknowledgements
This work was fully supported by the Research Grants Council of the Hong Kong Special Administrative Region, China, HKU 17108514References
1. Pantoni L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 2010;9(7):689-701.
2. Viswanathan A, Godin O, Jouvent E, et al. Impact of MRI markers in subcortical vascular dementia: A multi-modal analysis in CADASIL. Neurobiol Aging. 2010;31(9):1629-1636.
3. Vernooij MW, van der Lugt A, Ikram MA, et al. Prevalence and risk factors of cerebral microbleeds: The Rotterdam Scan Study. Neurology. 2008;70(14):1208-1214.
4. Chiang GC, Cruz Hernandez JC, Kantarci K, Jack CR, Weiner MW, Alzheimer’s Disease Neuroimaging Initiative for the ADN. Cerebral Microbleeds, CSF p-Tau, and Cognitive Decline: Significance of Anatomic Distribution. AJNR Am J Neuroradiol. 2015;36(9):1635-1641.
5. Poels MMF, Ikram MA, van der Lugt A, et al. Cerebral microbleeds are associated with worse cognitive function: The Rotterdam Scan Study. Neurology. 2012;78(5):326-333.
6. Rubinov M, Sporns O. Complex network measures of brain connectivity: uses and interpretations. Neuroimage. 2010;52(3):1059-1069.
7. Boisgueheneuc F du, Levy R, Volle E, et al. Functions of the left superior frontal gyrus in humans?: a lesion study. Brain. 2006;129(12):3315-3328.
8. Bruno JP, Sorter M, Arnold HM, Himmelheber AM. In Vivo Neurochemical Correlates of Cognitive Processes: Methodological and Conceptual Challenges. Rev Neurosci. 1999;10(1):25-48.
9. Apperly IA, Samson D, Chiavarino C, Humphreys GW, Humphreys GW. Frontal and Temporo-Parietal Lobe Contributions to Theory of Mind: Neuropsychological Evidence from a False-Belief Task with Reduced Language and Executive Demands. J Cogn Neurosci. 2004;16(10):1773-1784.
Figures