2375
White matter hyperintensity burden assessed ante-mortem and post-mortem on the same older adults1Department of Biomedical Engineering, Illinois Institute of Technology, Chicago, IL, United States, 2Rush Alzheimer's Disease Center, Rush University Medical Center, Chicago, IL, United States, 3Department of Neurological Sciences, Rush University Medical Center, Chicago, IL, United States, 4Department of Pathology, Rush University Medical Center, Chicago, IL, United States, 5Department of Diagnostic Radiology, Rush University Medical Center, Chicago, IL, United States
Synopsis
White matter hyperintensities (WMH) are commonly observed in brain MR images of older adults. Recently, more and more research studies assess WMH burden using ex-vivo MRI, aiming at directly linking WMH to the underlying neuropathologies detected at autopsy. The purpose of this work was twofold: 1) to investigate the relationship between WMH burden assessed in-vivo and ex-vivo on the same older adults, and 2) to test the hypothesis that WMH burden assessed ex-vivo is higher than that assessed in-vivo for longer ante-mortem intervals (AMI) (i.e. from in-vivo MRI to death).
Purpose
White matter hyperintensities (WMH) are commonly observed in brain MR images of older adults1. WMH are the result of neuropathology, which generally cannot be measured in-vivo. A number of in-vivo MRI studies have investigated the association of WMH burden with various risk factors2 to try to piece together the causes of WMH, and others have investigated the association of WMH burden with cognitive and motor outcomes3 to determine the clinical impact of WMH and the underlying neuropathologies. Recently, a number of studies have assessed WMH burden using ex-vivo MRI4, mainly aiming at directly linking WMH to the underlying neuropathologies detected at autopsy. These ex-vivo MRI investigations have a great advantage over in-vivo MRI investigations in that both MRI and histology assess the brain at the same condition, while in-vivo MRI is generally conducted months to years before death, and additional pathology (and WMH) may develop in the interval between imaging and death. On the other hand, all ex-vivo MRI investigations of WMH assume that WMH burden assessed ex-vivo is identical to that observed in-vivo, but that has not yet been established. Therefore, the purpose of this work was twofold: 1) to investigate the relationship between WMH burden assessed in-vivo and ex-vivo on the same older adults, and 2) to test the hypothesis that WMH burden assessed ex-vivo is higher than that assessed in-vivo for longer ante-mortem intervals (AMI) (i.e. from imaging to death).Methods
Participants and data acquisition:
83 community dwelling older adults (age: 90±7 years) were recruited from two longitudinal, cohort studies of aging. All participants underwent both in-vivo and ex-vivo MRI. In-vivo MRI included a T2-weighted FLAIR sequence (0.9x1.1x3 mm3 voxels) on a 1.5T and a 3T scanner. After death, a hemisphere was chosen from each participant and imaged ex-vivo approximately 30 days post-mortem, using a T2 multi-echo spin-echo sequence (0.6x0.6x1.5 mm3 voxels) and a T2-weighted FLAIR sequence (1.25x1.25x1.5 mm3 voxels) on a 3T scanner. The average ante-mortem interval (AMI) (from in-vivo MRI to death) was 2.2±1.5 years. The average post-mortem interval (PMI) (from death to immersion in fixative) was 8.1±4.7 hours.
In-vivo and ex-vivo WMH burden:
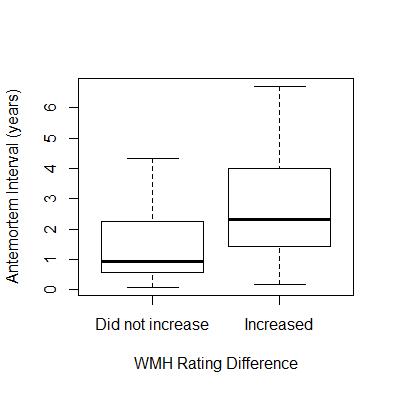
A rater was trained by an expert to rate the severity of periventricular and deep white matter WMH based on the original Fazekas scale (from 0 to 3). WMH burden was then defined as the maximum of the periventricular and deep white matter WMH ratings. Intra-rater reliability and agreement with the expert were assessed with intra-class correlation. The same process was repeated for both in-vivo and ex-vivo MR images of the same hemisphere. The in-vivo and ex-vivo ratings were compared for all participants. Also, two groups of participants were defined based on whether the WMH burden rating increased from in-vivo to ex-vivo MRI or not (excluding participants that had a maximum rating in-vivo), and logistic regression of two groups was used to test the hypothesis that increased WMH burden ex-vivo is associated with longer AMI.
Results
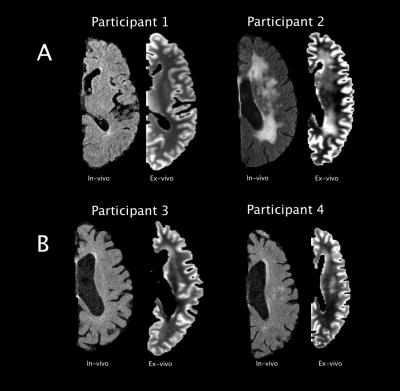
Intra-rater reliability and agreement with the expert were both strong, with ICC=0.76 and ICC=0.80, respectively). Overall, WMH burden generally stayed constant or increased from in-vivo to ex-vivo MRI (Fig.1). Figure 2 shows examples of in-vivo and ex-vivo images from such cases (Fig.2). Additionally, logistic regression showed that for every one year increase in AMI, the odds of greater WMH burden ex-vivo increase by 59% (p=0.04) (Fig.3).Discussion
The results of this study showed no drastic differences between in-vivo and ex-vivo WMH burden, providing strong evidence that WMH burden assessed ex-vivo is of the same nature as WMH burden assessed in-vivo. Any differences observed were due to additional pathology developing during the AMI. This is also in strong support of using ex-vivo MRI for assessing the neuropathologic correlates of WMH burden, as the in-vivo MRI findings and the amount of neuropathology measured at autopsy may not correspond to the same condition of the brain.Acknowledgements
National Institute of Neurological Disorders and Stroke (NINDS) UH2NS100599
National Institute on Aging (NIA) R01AG017917
National Institute on Aging (NIA) P30AG010161
National Institute on Aging (NIA) R01AG034374
References
1. Arvanitakis Z, Fleischman DA, Arfanakis K, et al. Association of white matter hyperintensities and gray matter volume with cognition in older individuals without cognitive impairment. Brain Struct Funct 2016;221;2135-2146.
2. Raz N, Yang Y, Dahle CL, Land S. Volume of white matter hyperintensities in healthy adults: contribution of age, vascular risk factors, and inflammation-related genetic variants. Biochim Biophys Acta 2012;3:361-369.
3. Silbert LC, Nelson C, Howieson DB, et al. Impact of white matter hyperintensity volume progression on rate of cognitive and motor decline. Neurology 2008;71:108-113.
4. Polvikoski TM, van Straaten EC, Barkhof F, et al. Frontal lobe white matter hyperintensities and neurofibrillary pathology in the oldest old. Neurology 2010;75:2071-2078.
Figures