2367
The Correlation of Olfactory Dysfunctions and Hippocampal Atrophy in Patients with Cognitive Impairment: A Potential Clinical Marker for Alzheimer’s Disease1Department of Radiology, Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China, NanJing, People's Republic of China, 2Department of Neurology, Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China, NanJing, People's Republic of China, 3Department of Radiology, Pennsylvania State College of Medicine, Hershey, PA, USA, Hershey, PA, United States
Synopsis
Olfactory deficits have been observed in subjects with Alzheimer’s disease (AD) and its potential as a biomarker has been demonstrated by several recent studies. However, its sensitivity and specificity in detecting early AD have not been validated in the Chinese population where aging population is growing rapidly. In this study, by using a 3.0 T MR scanner, we evaluate the presence of olfactory deficits and hippocampal volume loss measured by FreeSurfer (6.0) based on local population in China, to validate the use of olfactory test battery as a clinical AD marker.
Introduction
Olfactory deficits have been clearly observed in subjects with mild cognitive impairment (MCI) and Alzheimer’s disease (AD)1,2. Thus, its potential as a biomarker has been proposed and demonstrated by several recent studies 3,4. However, further validations of its sensitivity in detecting early AD and specificity in discriminating other neurodegenerative diseases are necessary with standardized cognitive assessments, concurrent olfactory tests and imaging evidence. In addition, these findings have not been validated in the Chinese population where aging population is growing rapidly. The goal of this study is to address these critical issues and to evaluate the presence of olfactory deficits and hippocampal volume loss based on local population in China.Methods
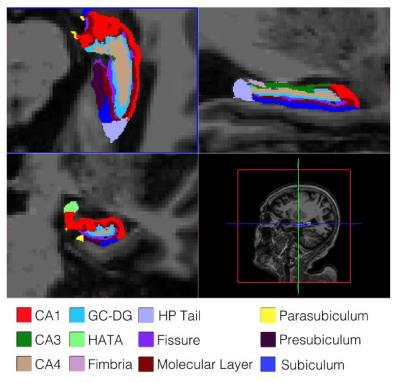
From June 2014 to January 2015, Sixty-one patients with memory complaints from Neurology Clinic of Drum Tower Hospital were recruited into this study. All the participants underwent a battery of neuropsychological tests for cognitive assessment. Thirty-one subjects and seven subjects were diagnosed with MCI and probable AD, respectively. Twenty-one subjects were considered as cognitively normal (CN)(figure 1). Olfactory test battery which included one trial of threshold test and one trial of identification test were performed by OLFACT-CTM (Osmic Enterprises, Inc., Cincinnati, Ohio, United States). Two patients with nausea of the odors were excluded from this analysis. Images were acquired on a 3 Tesla MR scanner (Achieva 3.0 T TX, Philips Medical Systems, Eindhoven, Netherlands) and a three-dimensional turbo fast echo (3D-TFE) T1WI sequence with TR/TE = 9.8/4.6 ms; filp angle = 8°; voxel size = 1.0×1.0×1.0mm3 was performed for volumetry analysis. Segmentation of hippocampal subfields were performed by the FreeSurfer (6.0) which divided the hippocampus into cornu ammonis (CA), dentate gyrus (DG), subiculum, presubiculum and other subfields (figure 2). Quantification of the subfields and estimation of total intracranial volume (TIV) were also calculated by the FreeSurfer for volumetry analysis.Results
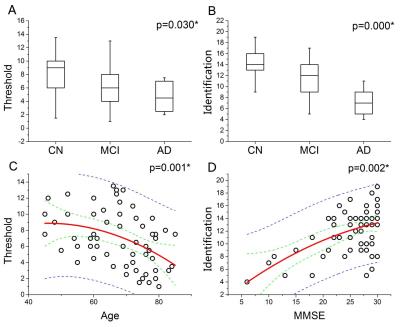
Increased olfactory threshold (p=0.030) and decreased ability of odor identification (p=0.000) were observed in the MCI and AD patients in compared with the CN subjects(figure 3). Partial correlation analysis indicated that olfactory threshold deficits was correlated with aging only (p=0.001) while odor identification impairment was correlated with both aging (p=0.011) and cognitive decline (p=0.002). Hippocampal volumetric analysis indicated significant atrophy of bilateral CA4 (both p<0.021) and presubiculum (both p<0.042) in the MCI and AD subjects. Asymmetric atrophy of left DG (p=0.030) and right parasubiculum (p=0.015) were also observed. After controlling for age, cognitive performances and TIV, partial correlation analysis suggested that odor identification dysfunction was correlated with atrophy of left CA4 (p=0.047) and left hippocampal fimbria (p=0.050), while no correlation of olfactory threshold deficits and hippocampal atrophy was found.Discussion
In compared with augmented olfactory threshold data in all three cohorts, results of odor identification test appear to be a relatively stable marker for AD detection. Volumetry analysis which indicated the correlation of odor identification dysfunction and hippocampal atrophy (left CA4 and fimbria) was in consist with such assumption. Based on our previous findings, no correlation between olfactory threshold deficit and hippocampal atrophy was also understandable since threshold decline was only correlated with normal aging. However, these findings and results were compromised by the limitation of sample size and the lack of objective assessment of the olfactory system. Further validations in follow-up studies of a larger cohort and objective analysis such as olfactory bulb imaging are needed.
We demonstrated that, in our Chinese cohort, a clear olfactory deficit in both MCI and AD compared to age-matched cognitively normal subjects, which indicated the use of olfactory test battery as a viable clinical marker for AD studies.
Acknowledgements
No acknowledgement found.References
1.Doty RL, Reyes PF, Gregor T, et al. Presence of both odor identification and detection deficits in Alzheimer's disease. Brain Res Bull. 1987; 18:597–600.
2.Doty RL.The olfactory vector hypothesis of neurodegenerative disease: Is it viable? Ann Neurol. 2008; 63:7–15.
3.Wang JL, Eslinger PJ, Doty RL, et al. Olfactory Deficit Detected by fMRI in Early Alzheimer’s Disease. Brain Res. 2010; 1357: 184–194.
4.Vasavada MM, Wang JL, Eslinger PJ, et al. Olfactory Cortex Degeneration in Alzheimer’s Disease and Mild Cognitive Impairment. Journal of Alzheimer’s Disease. 2015; 45: 947-958.
Figures