2357
Can EPVS reflect Cerebral Blood Flow and Cognitive State in MCI and AD Patients?1First Affiliated Hospital of Dalian Medical University, Dalian, People's Republic of China
Synopsis
EPVS may reflect underlying cerebral small vessel disease. We assumed the presence of EPVS were associated with cerebral blood flow (CBF)reduction ,and can accurately reflect the cognitive state.The study verifies a good coherence between EPVS and CBF in BG and CS of AD patients , and furthermore reflects of EPVS as the biomarker of cognitive status to a certain extent.
Objective
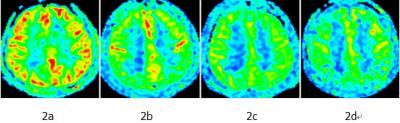
Enlarged perivascular spaces(EPVS)in the brain are common but generally overlooked and of uncertain pathophysiology. EPVS may reflect underlying cerebral small vessel disease. We assumed the presence of EPVS were associated with cerebral blood flow (CBF)reduction ,and can accurately reflect the cognitive state. In this study, arterial spin labeling (ASL) was used to analyze CBF changes in healthy volunteers and patients with MCI and AD;moreover correlation of EPVS、CBF in basal ganglia(BG)and centrum semiovale(CS)and MMSE were evaluated each other.Materials and Methods
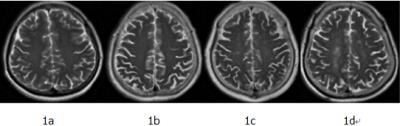
We recruited 39 patients:13 AD(MMSE<24),13 MCI(24≤MMSE<27)and 13 age-matched healthy volunteers as control (MMSE≥27). All subjects underwent 3D ASL sequence(PLD=1.5s) ,and then the ASL raw data was transferred to the ADW4.4 post-processing workstation to generate CBF map. The CBF values were manually measured in the bilateral BG and CS white matter (bilateral frontal and parietal lobes). The EPVS in BG and CS were observed and rated from score 1 to 4(Score 1 = 10, 2 = 11-20, 3 = 21-40, 4 => 40) on T2-weighted MRI. The t test was used to compare the CBF values between groups. The Kruskal-Wallis test and Kolmogorov-Smirnov Z test were used to compare the ranked data. Spearman correlation was used to analyze the relationship between EPVS scores, CBF and MMSE.Results
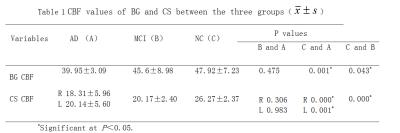
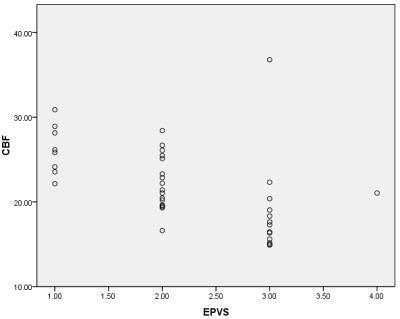
Paired sample t test showed there was significant lateral CBF values difference of CS (P=0.023), whileas no side difference of CBF values occurred on BG in AD patients ( P>0.05), in accordance with those in MCI patients and controls(Table 1). In comparison among the three groups the significant statistics difference of EVPS scores were found in both BG and CS (H values respectively =21.81,21.18, all P<0.01). In the BG, EPVS scores in AD group (2.15±0.68) was respectively higher than that in MCI(1.23±0.4)and NC group(1.07±0.27).In the CS, EPVS scores in AD group (2.76±0.59)and MCI group(2.38±0.50) were significantly higher than that in NC group(1.38±0.50)(P<0.01).Spearman correlation analysis showed that EPVS scores was negatively correlated to CBF values and MMSE in the BG (r=-0.399,-0.712, all P<0.01)and CBF values in the CS(r=-0.640, P<0.01)(Table 2).Discussion
This study used a convenient and feasible counting method. In AD patients, we found that the extent of EPVS in BG and CS was significantly higher than that in the controls. EPVS is a characteristic features of SVD, which frequently coexists with neurodegenerative disease, and can exacerbate cognitive deficits, physical disabilities, and so on. Cerebral small perforating vessels pathological changes can cause cerebral blood flow perfusion reduction. AS a result, EPVS and CBF in BG and CS were a good consistency .As the basal ganglia underwent language, memory, attention, spatial ability and other cognitive function, according to the results of this study, the EPVS in BG and MMSE scores were closely correlated, in coincided with the relative literatures.Conclusion
The study verifies a good coherence between EPVS and CBF in BG and CS of AD patients , and furthermore reflects of EPVS as the biomarker of cognitive status to a certain extent.Acknowledgements
No acknowledgement found.References
[1]: Wardlaw J M, Smith E E, Biessels G J, et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration[J]. Lancet Neurology, 2013,12(13):822-838.
[2]: Zhu Y C, Dufouil C, Soumaré A, et al. High degree of dilated Virchow-Robin spaces on MRI is associated with increased risk of dementia[J]. Journal of Alzheimers Disease Jad, 2010, 22(2):663-672.
Figures