2334
The effect of Amantadine on Persistent Vegetative State patients: an fMRI pilot study1Radiology & Psychiatry, Ichan School of Medicine at Mount Sinai, New York, NY, United States, 2Rehabilitation medicine, The First Hospital of Jilin University, Changchun, People's Republic of China, 3Radiology, The First Hospital of Jilin University, 4Radiology, Icahn School of Medicine at Mount Sinai, 5Icahn School of Medicine at Mount Sinai, 6Rehabilitation Medicine, The First Hospital of Jilin University
Synopsis
Task based fMRI and resting state scans were acquired on Persistent Vegetative State Patients before and after the administration of Amandatine. Significant clusters of activation was detected post treatment.
Introduction
There have been numerous studies that utilize fMRI to probe brain activity in comatose or persistent vegetative state (PVS) patients [1,2]. In these studies, fMRI has served as a metric for basal functional activity or as correlates with other metrics of consciousness. Amantadine HCL, a dopamine uptake blocker, has been used for the treatment of Parkinson's disease. It was also discovered to have beneficial effects on patients with disorders of consciousness with varying levels of success [3,4]. There have been limited fMRI studies on the effects of amantadine in PVS patients. Here we report on two patients who underwent fMRI before and after administration of amandatine.Methods
Two PVS patients who's families consented to the amantadine treatment were imaged using task driven and resting state fMRI. Patient 1 was a 53 yr old male who became vegetative after a car accident: Glasgow coma scale 8 and a level I on the Rancho Los Amigos rating scale. Patient 1 was imaged 105 days post injury. Patient 2 was a 10 yr old girl who was hit by a car: Glasgow Coma scale 9, level II on the Rancho Los Amigos scale and a 23 on the Disability Rating Scale. Patient 2 was imaged 70 days post injury.
Both patients were scanned on a Philips Ingenia 3T scanner using a 32 Ch headcoil and a Field Echo EPI sequence with sense acceleration: TR=2.5 seconds, TE=27ms, FOV=23cm, matrix size 96x96, slice thickness=2.5mm, 0 skip, 42 slices. The task driven acquisitions were block designs with 30 seconds on-off cycles. It was repeated 3 times with a total of 3 minutes and 30 seconds. The resting state scans were acquired using the same sequence for a total duration of 10 minutes. Patient 1 task fmri consisted of listening to a prerecorded voice of a close family member that was played back in segments of 30 seconds each with a 30 seconds silence as the control condition. During the second task fMRI the patient was told to visualize walking through a familiar environment (his house). For patient 2, a similar task was produced using a familiar voice of a family member. The second task was passive listening to a favorite childhood song split into 30 seconds epochs. Both patients received a 10 minutes resting state fMRI scan as well.
The above set of protocols were acquired and amandatine was administered and the protocols were repeated after approximately 15 mins and a second time after 2 or 4 hrs.
Task driven fMRI were analysed using Brain Voyager QX (Brain Innovation B.V. Maastricht, the Netherlands) and the resting state fMRI were processed using FSL Melodic (FSL. FMRIB Software Library. http://fsl.fmrib.ox.ac.uk/fsl/fslwiki/ ). All task fMRI figures thresholded at p<0.001.
Results
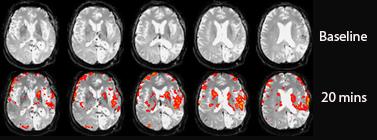
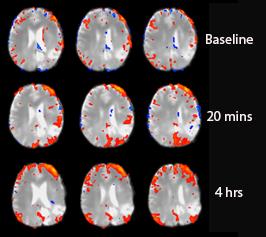
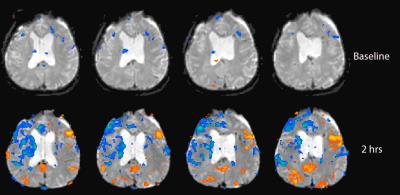
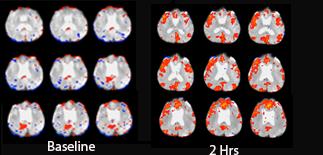
In both patients, significantly higher activity was detected after the administration of amandatine. In patient 1 significant increase in activity was detected in the motor and auditory cortex (Fig 1). The spatial navigation task also produced an increased activity but to a much lesser extent than the familiar voice scans. The resting state scan showed a significant increase in activity in the attention network after 20 mins and a more bilateral pattern after 4 hrs (Fig 2). In patient 2, the familiar voice produced a small increase in activity in parts of the insular cortex after amadatine. The most significant difference was with the favorite song task fMRI when imaged 2 hours post amandatine. Increased activity was detected in areas of the posterior cingulate, insular cortex, DLPFC and broca's areas (Fig 3). The baseline resting state fMRI scans did not show any clear known networks, but at 2 hrs after amandatine, an activity pattern that resembles the default mode network (Fig 4) as well as auditory networks appeared.Conclusion
Although these PVS patient's Glasgow Coma scale and Rancho Los Amigos scale did not change, we have shown a neurobiologic effect of amandatine in the short term. We are trying to follow these patients over a longer amandatine treatment period. These results warrant a larger scale study to investigate who might be potential responders to this type of treatment.Acknowledgements
No acknowledgement found.References
1) Owen AM, Coleman MR, Boly M, Davis MH, Laureys S, Pickard JDScience. 2006 Sep 8; 313(5792):1402.
2) Coleman MR, Davis MH, Rodd JM, et al. Towards the routine use of brain imaging to aid the clinical diagnosis of disorders of consciousness. Brain.2009;132:2541–2552.
3) Meythaler JM, Brunner RC, Johnson A, Novack TA. Amantadine to improve neurorecovery in traumatic brain injury associated diffuse axonal injury: a pilot double-blind randomized trial. J Head Trauma Rehabil 2002;17:300-13. 13.
4) Schneider WN, Drew-Cates J, Wong TM, Dombovy ML. Cognitive and behavioural efficacy of amantadine in acute traumatic brain injury: an initial doubleblind placebo-controlled study. Brain Inj 1999;13:863-72.
Figures