2260
High spatial resolution MRI-based three dimensional pathologic myopia eyes: a first step towards image-guided posterior sclera reinforcement1Department of MRI, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People's Republic of China, 2Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People's Republic of China, 3MR Research China, GE Healthcare, Beijing, People's Republic of China
Synopsis
Eyes of 66 high myopia patients who were to undergo posterior scleral reinforcement surgery (PSR) were examined by high-resolution three dimension cube magnetic resonance imaging. It is demonstrated that 3D MRI technique is helpful to PSR preoperative localization by comparing the precision rate of buckling strips position in groups with and without 3D MRI-guided. The present study demonstrates that it is possible to not only check the eyeball shape of the pathologic myopia patients accurately, but also assistant the PSR surgery by using 3D MRI technique.
PURPOSE
Posterior scleral reinforcement (PSR) is a surgical technique for pathologic myopia [1]. The shape and parameter of the pathologic myopia eyes were detected and measured by using three dimension magnetic resonance image (3D MRI) technique before and after PSR surgery. This study is to compare the precision rate of buckling strips position in pathologic myopia groups with and without high spatial resolution 3D MRI-guided.METHODS
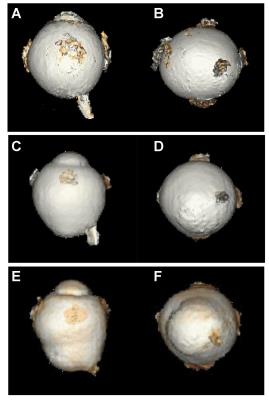
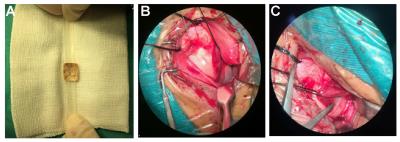
A total of 60 high myopia patients (myopic refractive error ≥-6.0 D) aged from 18 to 67 were recruited in this study including 30 patients undergone posterior sclera reinforcement with high spatial resolution 3D MRI-guided and 30 patients without 3D MRI-guided. All of the participants were examined with a GE Healthcare Discovery MR 750 3.0 T MRI scanner. To obtain high-contrast delineation of the edges of the eye, the following scanning sequences were performed: 3D T2-weighted CUBE sequence, which is an improved sequence of 3D fast-spin echo, with the following parameters: TR=2500.0 ms, TE=90ms,section thickness=1.0mm with a 0 mm section gap, layer=128, echo train length (ETL) =90, FOV= 256mm×230mm,matrix= 320×320. Volume render of the images from 3D data were done by computer workstation (AW 4.5). And the eyeballs were reconstructed. The two distances, from the temporal limbus cornea to the temporal border of the staphyloma and from the temporal border of the staphyloma to the temporal border of the optic nerve, were measured on the 3D eyeball imaging in the MRI workstation (Fig. 1). The reinforcement materials were reconstructed after PSR surgery by 3D MRI (Fig. 2).RESULTS
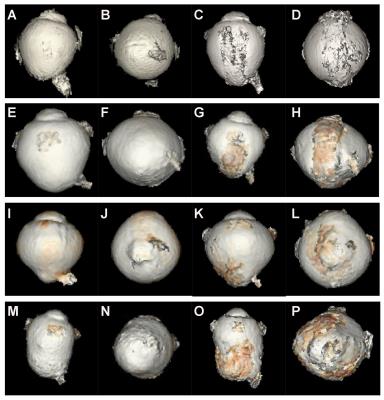
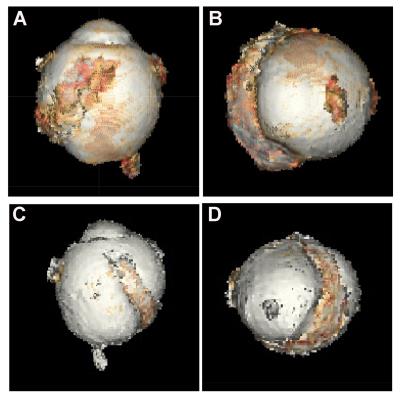
Two ophthalmologists and two MRI experts divided the pathologic myopia eyeballs into three types, including the macular staphyloma group (15 patients, 25%), optic staphyloma group (28 patients, 46.7%) and no posterior staphyloma group (17 patients, 28.3%) (Fig.3). The two distances measured were helpful for the ophthalmologist in the material preparation and the posterior sclera reinforcement (Fig.4). All the reinforcement materials were under the exact macular area in group 1 guided by 3D MRI (as shown in Fig.5A, 5B). The silicone bands of patients in group 2, 22 (73.3%) out of 30 were under the exact macular area, 8 (26.7%) of 30 slid to the temporal side of the macular area (as shown in Fig.5C,5D).DISCUSSION
High myopia is characterized by axial eye elongation and thinning of the posterior sclera, likely resulting from the weakening of the biomechanical properties of sclera [2]. Surgeons seek to prevent axial elongation and staphyloma progression by the placement of grafts over the posterior. PSR surgery was first reported by Shevelev in 1930[3]. It was described to be the only effective method that can delay or stop the progression of high myopia [4,5]. The posterior sclera staphyloma was divided into three types in this study., The staphyloma could be covered completely by a narrow strip easily, due to the macular staphyloma is far from the optic nerve compared with the optic staphyloma. In other word, the risk of the damage to the optic nerve is small due to the long distance and the narrow band. It noted that the PSR surgery in group 2 mimicked the traditional protocol in the previous study. The clue of the previous PSR failure was clearly shown in this study.CONCLUSION
The posterior sclera staphyloma, for the first time, were clearly presented by using 3D MRI technique. This study showed the shape of staphyloma before and after the surgery. It is important for a successful surgical with the personalized design of the reinforcement strip guided 3D cube MRI. The present study demonstrates that it is possible to not only check the eyeball shape of the pathologic myopia patients accurately, but also assistant the PSR surgery by using 3D MRI technique.Acknowledgements
No acknowledgement found.References
1. Xue, A., et al., Posterior scleral reinforcement on progressive high myopic young patients. Optom Vis Sci, 2014. 91(4): p. 412-8.
2. McBrien, N.A., A.I. Jobling, and A. Gentle, Biomechanics of the sclera in myopia: extracellular and cellular factors. Optom Vis Sci, 2009. 86(1): p. E23-E30.
3. MM., S., Operation against high myopia and scleralectasia with aid of the transplantation of fascia lata on thinned sclera. Russian Oftalmol 1930. 11: p. 107-110.
4. Ward, B., E.P. Tarutta, and M.J. Mayer, The efficacy and safety of posterior pole buckles in the control of progressive high myopia. Eye (Lond), 2009. 23(12): p. 2169-2174.
5. Gerinec, A. and G. Slezakova, Posterior scleroplasty in children with severe myopia. Bratisl Lek Listy, 2001. 102(2): p. 73-78.
Figures