2259
Quantitative analysis of shape of eyes with high myopia by high-resolution three-dimensional magnetic resonance imaging1Department of MRI, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People's Republic of China, 2MR Research China, GE Healthcare, Beijing, People's Republic of China, 3Department of Ophthalmology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People's Republic of China
Synopsis
Myopia is a major cause of blindness worldwide. 134 patients with high myopia and 120 emmetropic volunteers were examined. All of the participants were scanned by high resolution 3D T2-weighted CUBE MRI sequence. This study is to evaluate the preoperative localization and postoperative assessment value of high-resolution 3D MRI for high myopia. It is shown that the axial length, horizontal length, vertical length and volume of the high myopia were significantly longer than those of the emmetropia. And high resolution 3D MRI could clearly demonstrate the position of staphylomas, superior rectus, inferior rectus, medial rectus, lateral rectus and optic nerve.
PURPOSE
As the most familiar eye disorder, the prevalence rate of myopia has increased noticeable in the past decades in many regions of the world [1] . High myopia is a major cause of legal blindness worldwide and characterized by an abnormal shape of the eye, which usually form a posterior staphyloma [2]. Posterior scleral reinforcement (PSR) surgery is a potential treatment method for high myopia [3]. Precisely describe the abnormal shape of the eyes and display the position relationship of staphyloma and rectus would be important for preoperative preparation. In this study, we would like to gain the geometric characteristics of the posterior staphyloma in high myopia by high resolution three-dimensional (3D) magnetic resonance imaging (MRI). And display the position of the superior rectus, inferior rectus, medial rectus and lateral rectus to assist the preoperative preparation.METHODS
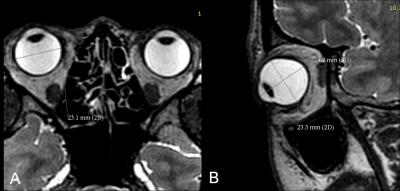
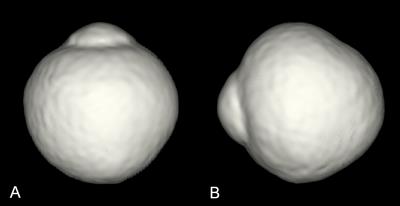
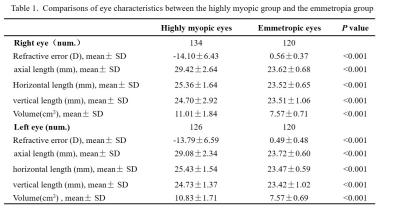
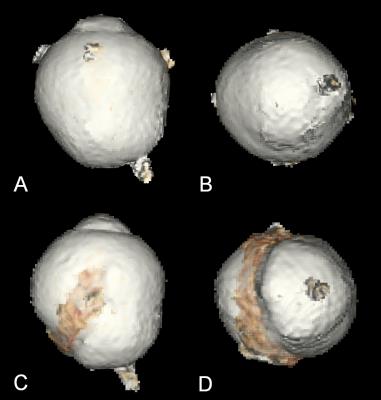
134 high myopia patients (myopic refractive error ≥-6.0 D) and 120 emmetropic normal controls were recruited in this study. Firstly, all of the participants were examined with a 3.0T MRI scanner (Discovery MR 750; GE Medical Systems, Milwaukee, WI, USA) using an improved sequence of 3D fast-spin echo named 3D T2-weighted CUBE sequence, which was performed to obtain high contrast delineation of the edges of the eye with the following parameters: TR=2500ms, TE=90ms, section thickness=1.0mm with a 0 mm section gap, layer=128, echo train length (ETL) =90, FOV=256mm×230mm,matrix= 320×320. The scan time for each subject was 3 minutes 18 seconds. Secondly, axial length, horizontal length, vertical length of the eyeball were measured (Fig.1). Volume renderings of the 3D MRI images were then performed by computer workstation and the volume of the eyeball was measured (AW 4.5) (Fig. 2). The differences in the axial length, horizontal length, vertical length, and volume of the eyeball between high myopia and emmetropia group were tested by student’s t test. Finally, 16 patients of 134 high myopia were to undergo surgery and the scleral strip of PSR were observed by 3D MRI after operation (Fig. 3). All statistical analyses were performed by SPSS 16.0 (SPSS Inc., Chicago, IL, USA). A two-sided P value less than 0.05 was considered as the significant level.RESULTS
The results showed the axial length, horizontal length, vertical length and volume of the high myopia were significantly longer than those of the emmetropia (Table 1). Among 223 eyes of staphylomas, 145 cases happened in temporal side, 32 in nasal side and 46 in peripapillary. And the positon of the superior rectus, inferior rectus, medial rectus, lateral rectus and optic nerve were demonstrated in the reconstructed images after eyeballs image segmentation (shown in Fig.4).DISCUSSION
High myopia is characterized by an abnormal shape of the eye, for example an excessive axial elongation of the globe and the formation of posterior staphyloma. The results about geometric characteristics of high myopia significantly larger than the emmetropic ones, and the axial length obviously increasing more than the vertical length and the horizontal length in present study were also observed in Vohra’s paper [4]. But, the result about staphyloma happening in temporal side went against Moriyama’s research [5]. The reasons for that are unclear, probably because of the composition of the patients or ocular physiological anatomy. Ophthalmologist perform PSR surgery which remains a rational treatment method to prevent the progression of pathological myopia. Accurate location of rectus and optic nerve through 3D MR image before operation can provide more information to PSR surgery [6]. At the same time, ophthalmologists could get the exact positions of the scleral strip, so that reinforcement band could surround the staphyloma exactly and be anchored in place to the sclera.CONCLUSION
It is demonstrated that 3D MRI not only can clearly show the geometrical parameters of eyeball, position of the staphyloma, recti and optic nerve attachment to the eyeball and the geometrical information for PSR preparation, but also reflect the fact of the scleral strip after PSR surgery. 3D MRI may become an effective technique in PSR preoperative location and postoperative assessment according to this study.Acknowledgements
No acknowledgement found.References
1. Bar Dayan, Y., et al., The changing prevalence of myopia in young adults: a 13-year series of population-based prevalence surveys. Invest Ophthalmol Vis Sci, 2005. 46(8): p. 2760-5.
2. He, M., et al., Refractive error and visual impairment in urban children in southern china. Invest Ophthalmol Vis Sci, 2004. 45(3): p. 793-9.
3. Thompson, F.B., A simplified scleral reinforcement technique. Am J Ophthalmol, 1978. 86(6): p. 782-90.
4. Vohra SB, Good PA. Altered globe dimensions of axial myopia as risk factors for penetrating ocular injury during peribulbar anaesthesia. Br J Anaesth. 2000; 85:242-245.
5. Moriyama M, Ohno-Matsui K, Hayashi K, et al. Topographic analyses of shape of eyes with pathologic myopia by high-resolution three-dimensional magnetic resonance imaging. Ophthalmology. 2011;118:1626-1637.
6. Yan Z, Wang C, Chen W, Song X. Biomechanical considerations: evaluating scleral reinforcement materials for pathological myopia. Can J Ophthalmol. 2010;45:252-255.
Figures