2246
Gray matter reduction is associated with poor treatment response in patients with schizophrenia: A voxel-based morphometry study with a strict control of multiple clinical variables1Institute of Medical Device and Imaging, National Taiwan University College of Medicine, Taipei, Taiwan, 2Department of Psychiatry, National Taiwan University Hospital, Taipei, Taiwan, 3Graduate Institute of Brain and Mind Sciences, National Taiwan University College of Medicine, Taipei, Taiwan, 4Department of Medical Imaging, National Taiwan University Hospital, Taipei, Taiwan, 5Molecular Imaging Center, National Taiwan University, Taipei, Taiwan
Synopsis
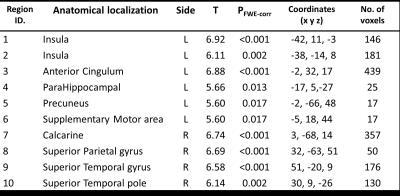
To investigate whether remitted and non-remitted patients with schizophrenia had distinctly different gray matter volumes, we used voxel-based morphometry (VBM) to analyze group difference by controlling all possible clinical variables. As compared with remitted patients, the non-remitted patients showed 10 brain areas with significantly decreased gray matter volume. Our results imply that remitted and non-remitted patients might have distinct patterns of gray matter reduction, and the characteristics of gray matter change might represent the structural correlate of treatment response in patients with schizophrenia.
Introduction
Long-term treatment outcome has been considered to associate with brain structure alterations. Molina et al. found a significant decrease in subcortical gray matter volumes in patients with poor outcome as compared with those with good outcome (Molina et al., 2010). However, previous studies on schizophrenia also found gray matter volume reduction in association with antipsychotic exposure (Ho et al., 2011) and duration of illness (Chan et al., 2009). In other words, potential effects of the clinical variables on gray matter volume should be controlled when investigating the association between brain structure alterations and treatment outcome. Therefore, this study investigated the difference in gray matter volume between remitted and non-remitted patients by adjusting multiple clinical variables, i.e. age, sex, duration of illness and dose of antipsychotic medication, in a large sample of patients.Methods
We recruited 68 remitted patients with schizophrenia (male/female = 28/40, age = 31.47±7.75 years), 47 non-remitted patients with schizophrenia (male/female = 25/22, age = 34.6±9.63 years) in this study. Patients were assessed according to the Positive and Negative Syndrome Scale (PANSS) scores after the treatment (Andreasen et al., 2005). Remission was defined as having a score of 3 or less on each of eight specific items in PANSS (i.e. P1, P2, P3, N1, N4, N6, G5, G9), otherwise, non-remission. All subjects were scanned on a 3T MRI system (TIM Trio, Siemens, Germany). High resolution T1-weighted images were acquires using a three-dimensional magnetization prepared rapid gradient echo (3D MPRAGE) sequence with the following parameters: TR = 2000 ms, TE = 3 ms, flip angle = 9°, acquisition matrix = 256 × 192 × 208, FOV = 256 × 192 × 208 mm3, resolution = 1 x 1 x 1 mm3. Data was analyzed using a voxel-based morphometry (VBM) approach (SPM 12b, Wellcome Trust Centre of Neuroimaging, www.fil.ion.ucl.ac.uk). Gray matter volumes were compared between the two groups using voxel-wise analysis, ANCOVA with total gray matter volume as well as age, sex, duration of illness and dose of antipsychotic medication as covariates. Groups were compared using t-contrast with statistical threshold set to p<0.05 with the family-wise error rate correction, and cluster size bigger than 10 contiguous voxels. Coordinates of significant regions were referred to anatomic structures using AAL atlas.Results
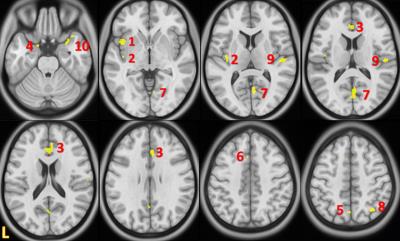
Non-remitted patients showed gray matter volume reduction in multiple areas in the left hemisphere including the insula, anterior cingulum, parahippocampal, precuneus and supplementary motor area, and in the right hemisphere including the calcarine, superior parietal gyrus, superior temporal gyrus and superior temporal pole (Table 1 and Figure 1). In contrast, there was no gray matter volume increase in the non-remitted patients.Discussion
To the best of our knowledge, this is the first study to confirm gray matter volume difference between remitted and non-remitted patients with schizophrenia in a large sample of subjects and a strict control of multiple clinical variables. With respect to the remitted patients, the non-remitted patients showed multiple brain areas with significantly decreased gray matter volume. Our results imply that remitted and non-remitted patients might have distinct patterns of gray matter reduction, and the characteristics of gray matter change might represent the structural correlate of treatment response in patients with schizophrenia.Acknowledgements
No acknowledgement found.References
1. Fusar-Poli, P., et al (2013). Neuroscience & Biobehavioral Reviews, 37(8), 1680-1691.
2. Olabi, B., et al (2011). Biological psychiatry, 70(1), 88-96.
3. Andreasen, N. C., et al (2011). Biological psychiatry 70(7), 672-679.
4. Molina, V., et al (2010). Psychiatry Research: Neuroimaging, 184(1), 16-22.
5. Ho, B.C., et al (2011). Arch. Gen. Psychiatry 68, 128–137.
6. Chan, R. C., et al (2011). Schizophrenia bulletin, 37(1), 177-188.
7. Andreasen, N. C., et al (2005). American Journal of Psychiatry 162(3), 441-449.
Figures