2199
Proton MR spectroscopy detection of high lipid levels without central necrosis and high intensity on DWI is characteristics of germinomaFumiyuki Yamasaki1, Yasuyuki Kinoshita1, Satoshi Usui1, Takeshi Takayasu1, Ryo Nosaka1, Manish Kolakshyapati1, Taiichi Saito1, Kazuhiko Sugiyama2, and Kaoru Kurisu1
1Neurosurgery, Hiroshima University, Hiroshima, Japan, 2Clinical Oncology & Neuro-oncology Program, Hiroshima University Hospital, Hiroshima
Synopsis
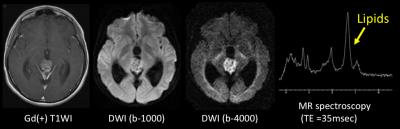
MRS and DWI of germinoma
Background
Background: The differentiation of germinoma from other tumors by conventional magnetic resonance (MR) imaging can be very difficult. Advanced imaging findings of germinoma have not been well documented. The purpose of our study was to determine if advanced MR imagings could give additional information for definitive diagnosis of germinoma.Materials and methods
Our institutional review board approved this retrospective study. We retrospectively reviewed the images of 27 histologically confirmed germinoma patients treated in our institution between Oct 2004 and November 2016. We also studied 23 patients with pineal tumors which included 11 non-germinomatous germ cell tumors (NGGCT), 9 pineal parenchymal tumors [3 pineocytoma, 3 pineal parenchymal tumor of intermediate differentiation (PPTID), 3 pineoblastoma], 2 meningioma, 1 anaplastic astrocytoma. All patients underwent conventional MR imaging and advanced MR imaging including diffusion-weighted imaging and/or single voxel proton MR spectroscopy.Results
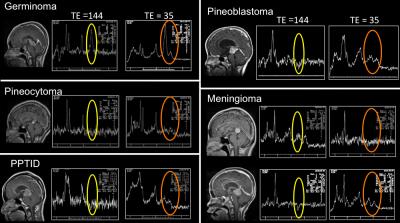
In germinoma patients group, age ranged from 9 to 37-years (average 16.9, median 14). 24 were male, and 3 were female patients. 17 patients had single lesion, while 10 had multiple lesions including 3 with disseminated diseases. Bithalamic extension was observed in 12 of 18 patients with pineal germinoma, but only 5 of 12 patients showed edema at thalamus. The cyst formation was observed in 13 of 27 patients. 11 of 21 examined tumors showed high intensity on diffusion-weighted imaging. High lipids peak at single voxel proton MR spectroscopy was observed in 15 of 15 examined tumors. On the other hand, in the pineocytoma, PPTID, pineoblastoma, meningioma and anaplastic astrocytoma, lipid peaks were small or absent. In NGGCT group, high lipids peak at single voxel proton MR spectroscopy was also observed in 11 of 11 examined tumors, however, they did not show high intensity on DWI rather they showed low to high mixed intensity. Representative case of germinoma was shown in figure 1. Representative proton MR spectroscopy results were shown in figure 2.Discussion
Lipid signals in most brain tumors can be observed when the spectra are acquired at TE shorter than 50 ms. Mobile lipid resonances are generally observed in contrast-enhancing and necrotic areas of the tumor. Brain tumors tend to be profoundly heterogeneous and include areas of viable tumor, necrosis, and hemorrhage. Elevated lipid peaks were considered a characteristic of high grade tumor with central necrosis. However, a recent study demonstrated that high lipid peaks in tumors without central necrosis are a characteristic of malignant lymphomas (1). It has been suggested that the detection of high lipid peaks in malignant lymphomas reflects a high cell turnover and infiltration by macrophages (2). Histologically, germinoma exhibits two-cell-pattern composed of tumor cells and infiltrated lymphocytes. High lipids peak in germinoma may reflect lymphocyte in tumor cells, which is the characteristics of germinoma. This infiltrated lymphocytes result in high cellularity in germinoma, which in turn results in low ADC and high intensity on DWI.Conclusion
High intensity on diffusion-weighted imaging and high lipids peak at single voxel proton MR spectroscopy are characteristics of germinoma.Acknowledgements
No acknowledgement found.References
(1) Yamasaki F, Takayasu T, Nosaka R, Amatya VJ, Doskaliyev A, Akiyama Y, Tominaga A, Takeshima Y, Sugiyama K, Kurisu K: Magnetic resonance spectroscopy detection of high lipid levels in intraaxial tumors without central necrosis: a characteristic of malignant lymphoma. J Neurosurg 122: 1370-1379, 2015
(2) Hermann M, Niemitz C, Marafioti T, Schriever F: Reduced phagocytosis of apoptotic cells in malignant lymphoma. Int J Cancer 75: 675-679, 1998