2162
1H MAGNETIC RESONANCE IMAGING OF THE LUNGS USING PROPANE AS AN INHALATION AGENTAshlyn Kopanski1, Francis Hane2, Tao Li1, and Mitchell Albert3
1Lakehead University, Thunder Bay, ON, Canada, 2Lakehead University, MURILLO, ON, Canada, 3Thunder Bay, ON, Canada
Synopsis
We used 80% propane/20% oxygen mixture as an imaging agent and conventional 1H MRI to image the lungs of a living rat. We believe that this is the first time propane gas has been used in vivo for imaging of the lungs. We obtained an SNR approaching 50 from the propane in the lungs. Our results demonstrate that propane has a possibility of being used as a lung imaging modality for detection of various pulmonary diseases.
Purpose
Magnetic resonance imaging (MRI) of the lungs is inherently problematic because the lungs are in constant motion and have little 1H density. To overcome these challenges associated with lung imaging, a variety of inhalation magnetic resonance agents have been developed such as hyperpolarized (HP) noble gases and inert fluorinated gases (1, 2).. Both of these methods require specialized multinuclear coils and MRI system and a polarizer for HP gases. This work demonstrates the use of propane as an inhalation agent for 1H imaging the lungs of a living rat. We achieved a useable signal noise ratio (SNR) approaching 50. This method may be used in the future to assist in the diagnosis, staging, and treatment of a wide variety of pulmonary diseases at a fraction of the cost of HP gases.Methods
Sprague-Dawley rats (n=6) were placed into the custom 1H RF coil within the bore of the Philips Achieva 3T whole-body scanner operating at the 1H resonance frequency of 127.73 MHz. The rat vas ventilated with 100% O2 via the endotracheal tube using the custom-built rat ventilator. Prior to propane enhanced image acquisition, the rat was continuously ventilated with a 80% propane/20% oxygen mixture. TSE projection images were then acquired with a field of view of 150 mm x 150 mm with a matrix size of 256 x 256 and an in-plane resolution of 0.58 mm, 18 mm slice thickness, TR = 2 s, TE = 40 ms, 90° flip angle, bandwidth 300 Hz/pixel, NSA=6. TSE projection images were acquired both with the rat ventilated with a mixture of 80% propane/20% oxygen and with the rat ventilated with pure oxygen. Following the image acquisition, the “oxygen” images were subtracted, voxel-by-voxel, from the raw “propane” images to obtain an effective “propane” (i.e. propane enhanced) image.Results and Discussion
Propane associated MRS peaks were not differentiated from endogenous signal peaks given the large proton concentration. We obtained an SNR of 47.5 by subtracting the “oxygen-only” image from the “propane” image. This image was thresholded and segmented for image clarity and overlayed on a conventional MR image of the thorax (Figure 1). To ensure our “subtraction” method of imaging was in fact capturing a higher signal within the lungs of the rat, an “inversion” image was processed which revealed the lungs to be dark (Figure 2). This demonstrates the robustness of our image processing methodology.Conclusion
By continuously ventilating the rats with a 80% propane/20% oxygen mixture (800,000 ppm propane) for periods of up to 20 minutes, no adverse health effects were observed. These rats were not recovered after experiments so any long-term health effects were unable to be determined at this time. We believe that these data are the first report of in vivo applications of propane as an imaging agent of the lungs in a live animal model. Our SNR measurements were comparable to those of fluorinated gases which demonstrates the feasibility of propane gas as a lung imaging modality for the detection of pulmonary diseases.Acknowledgements
FH hold fellowships from the BrightFocus Foundation and the Canadian Institutes for Health Research. FH wishes to thank the BrightFocus Foundation and their generous donors for their support. AK holds an undergraduate research award from the Natural Sciences and Engineering Research Council.References
1. Albert MS, Cates GD, Driehuys B, et al.: Biological magnetic resonance imaging using laser-polarized 129Xe. Nature 1994:199–201.
2. Couch MJ, Blasiak B, Tomanek B, et al.: Hyperpolarized and Inert Gas MRI?: The Future. Mol Imaging Biol 2014.
Figures
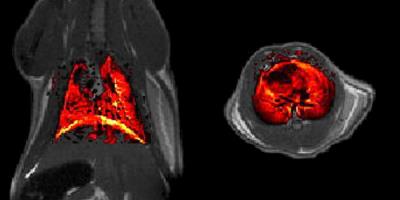
Propane enhanced MR image (coronal-left, axial-right)
overlaid on the underlying high resolution anatomical MR image. The enhanced
propane image was registered, thresholded and segmented for image clarity.

“Inverse” propane enhanced MR image created by the
subtraction of normal breathing rat MR image from a propane breathing rat MR
image. Notice the body is bright while the lungs are dark.