2159
Human Lung Morphometry using Hyperpolarized 129Xe Multi-b Diffusion MRI with Compressed Sensing1School of Physics, Huazhong University of Science and Technology, Wuhan, People's Republic of China, 2Key Laboratory of Magnetic Resonance in Biological Systems, State Key Laboratory of Magnetic Resonance and Atomic and Molecular Physics, National Center for Magnetic Resonance in Wuhan, Wuhan Institute of Physics and Mathematics, Chinese Academy of Sciences, Wuhan, People's Republic of China, 3Department of Magnetic Resonance Imaging, Zhongnan Hospital of Wuhan University, Wuhan, People's Republic of China
Synopsis
This work is to investigate the feasibility of compressed sensing (CS) on the morphologic measurement of lung microstructure using hyperpolarized 129Xe diffusion magnetic resonance imaging (MRI). The fully sampled (FS) and prospective CS multi-b diffusion MRI data were obtained from five healthy subjects and one COPD patient, respectively. The maps and global average values of mean linear intercept length (Lm) were calculated using cylinder model. The results were compared between FS and CS method for all subjects. The difference between FS and CS ranged from -2.3% to 7.2%. A highly Person’s correlation (R=0.988) between FS and CS was presented.
Purpose
To investigate the feasibility of compressed sensing (CS) on the morphologic measurement of lung microstructure using hyperpolarized 129Xe diffusion MRI.Introduction
129Xe diffusion MRI is sensitive to acinar airway. Combined with the simplified models such as Weibel model and theoretical methods (1), multi-b diffusion MRI method can offer the information of lung structure at the alveolar level. However, this needs a long scanning time. In this work, we develop a new method combining multi-b diffusion MRI with CS (2) to accelerate the acquisition in order to measure microstructure of human lungs.Methods
Fully sampled (FS) and undersampled 129Xe multi-b diffusion MRI data were acquired from five healthy subjects and one COPD patient, respectively. The parameters of 2D spoiled gradient echo sequence were as follows: FOV = 384*384 mm2, TR/TE = 13.9/10.9 ms, matrix = 64*64, number of slices = 4, slice thickness = 30 mm, coronal slices, receiver bandwidth = 250 Hz/pixel, flip angle = 5°, centric phase encoding direction. The bipolar diffusion weighting gradient pulse was as follows: ramp up/down time = 0.3 ms, duration time = 3.7 ms, diffusion time Δ = 5 ms, b = 0, 10, 20, 30, 40 s/cm2, the diffusion gradient were located on the slice selection direction. The parameters of the prospective CS acquisition were the same as those of FS except that the phase encoding number reduced to 32 and the flip angle raised from 5°to 7°. In this work, we used the pseudo-random pattern for two-fold undersampling in phase direction. A nonlinear method was used to enforce the sparsity using the L1 norm (3). The reconstruction of the image involves solving equation minx1/2||Fu-y||22+λ1||Ψx||*+λ2TV(x). The maps of mean linear intercept length (Lm) were calculated using cylinder model, Lm map and global mean Lm of CS were compared with those of FS for all subjects. The scatter and Bland-Altman plots were used to verify the agreement between CS and FS measurements.Results and Discussion
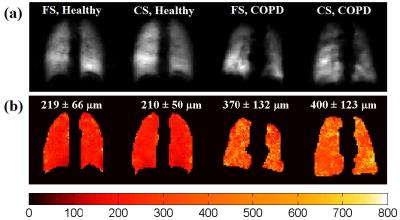
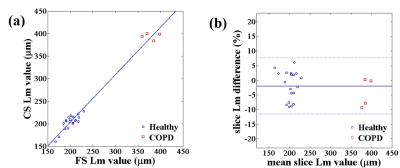
Figure 1 showed the ventilation images of b=0 and Lm maps of one healthy subject and the COPD patient by FS and CS, respectively. In the chosen example slices, some ventilation defect regions could be observed obviously in the ventilation images of the COPD patient. There were generally some differences in lung sizes and positions between FS and CS acquisition, and the differences became more obvious for COPD patient, because two acquisitions were obtained in different breath-holds. The differences in mean Lm of healthy and COPD subjects between FS and CS were 9 μm (4.1%) and 30 μm (8.1%) respectively. The mean Lm difference of the COPD patient was larger than that of the healthy subject, which was in accordance with the difference of ventilation images. The scatter plot and Bland-Altman analysis plot about the slice-by-slice Lm values between FS and CS methods were showed in Figure 2. A good correlation (R = 0.988) was observed (Fig. 2a), and all points fell within the 95% confidence intervals in the Bland-Altman plot (Fig. 2b). The mean Lm percent difference between methods was -1.9%. And 95% of the difference fell within -11.5% to +7.7%. In the quantitative comparisons of Lm, two clusters of data points were observed corresponding to the healthy and COPD groups. The results suggested that the CS method could also be used to extract the pulmonary parameters accurately with the twice shorter time in comparison to the FS method.Conclusions
In this study, we demonstrated that the multi-b diffusion with CS method is a promising accelerated technique to obtain the lung morphometric parameters in a single breath hold. Our results showed that lung morphometric parameters using prospective CS are in agreement with that of the FS images. This provides confidence for the use of 129Xe lung morphometry to detect changes of lung diseases.Acknowledgements
We acknowledge the support by the National Natural Science Foundation of China (81227902, 81625011) and National Program for Support of Eminent Professionals (National Program for Support of Top-notch Young Professionals).References
1. Magn Reson Med 2012 67(3):856-866.
2. Ieee Transactions on Information Theory 2006 52(2):489-509.
3. Ieee Transactions on Information Theory 2006 52(4):1289-1306.
Figures