2139
Rapid acquisition of co-registered 3D xenon-129 and proton images of the human lung in a single breath-hold using compressed sensing1Academic Unit of Radiology, University of sheffield, Sheffield, United Kingdom
Synopsis
The feasibility and suitability of using compressed sensing to accelerate the acquisition of 3D lung ventilation images with hyperpolarized 129Xe and to enable same-breath anatomical 1H imaging was investigated. Fully sampled and prospective data were acquired from one healthy smoker. Retrospective simulations showed a good agreement between fully sampled and reconstructed images using different error metrics. The method was further validated by comparing quantitative imaging metrics; percentage ventilated volume, distribution of signal intensity and maps of coefficient of variation in prospectively acquired data. The results indicate that the method can be implemented for clinical evaluation in patients with lung diseases.
Purpose
Lung ventilation MRI with hyperpolarized (HP) gases (3He and 129Xe) has been shown to be sensitive to different obstructive lung diseases (e.g. chronic obstructive pulmonary disease, cystic fibrosis, asthma). Same-breath acquisition of HP 3He ventilation images and anatomical 1H images provides a reproducible method to derive sensitive markers such as percentage lung ventilation (%VV) measurement.1 With the limited supply and rising cost of 3He gas, 129Xe provides a cost-effective alternative to 3He 2, but due to its lower gyromagnetic ratio, lower bandwidths are required to obtain reasonable SNR, which increases the acquisition time. Therefore, same-breath whole lung coverage acquisition of HP 129Xe ventilation and 1H anatomical images has not yet been feasible for clinical imaging in patients and retrospective registration of separate breath HP 129Xe and 1H images is required.2,3 Compressed Sensing (CS) 4 has been successfully applied to accelerate the acquisition of HP gas ventilation images 5 and to enable same breath 3D 3He and 1H imaging.6 In this work, CS techniques were used to accelerate the acquisition of 3D 129Xe ventilation images and enable same-breath acquisition of co-registered anatomical 1H images.Methods
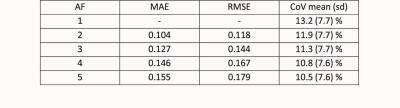
A fully sampled (FS) 3D HP 129Xe ventilation dataset was acquired on a GE HDx 1.5T MR scanner (using 800 mL of 129Xe at ~25% polarization, 7 mixed with 200 mL of N2) from one healthy smoker (male, 31 years, FEV1 z-score>-1.64) in order to perform retrospective CS simulations and optimize the undersampling scheme. Imaging parameters were: 3D balanced steady-state free-precession 8 pulse sequence with elliptical-centric encoding, 96x78x32 matrix, FOV: 40x32.5x24 cm3, TE/TR: 3.6/7.6 ms, bandwidth: ±8.06 kHz, scan time of 19 s. Elliptical-centric encoding strategy was chosen for both FS and subsequent prospective under-sampled acquisitions in order to maximise image SNR. CS-reconstruction fidelity was evaluated with different image metrics including mean absolute error (MAE) and root mean square error (RMSE) of signal intensity in the original size images and pixel-by-pixel comparison in the segmented ventilated volume of the DICOM images (256x256x32 matrix). Coefficient of variation (CoV) of the ventilated lung 9 was also evaluated. After CS optimization, additional 3D FS and CS accelerated prospective acquisitions (acceleration factor AF = 3) of both HP 129Xe and 1H data were acquired in the same breath-hold. The anatomical 1H sequence was a fast spoiled gradient echo with the same resolution as the HP 129Xe ventilation image but with a square in-plane FOV of 40x40 cm2 (TE/TR: 0.6/1.9 ms, bandwidth: ±83.3 kHz, partial Fourier encoding in the frequency direction of 0.8 and acquisition time of 6 s). %VV values and CoV maps from FS and CS datasets were calculated using a semi-automated segmentation software 10 and compared. Additionally, both CS and FS HP 129Xe ventilation images were registered to each other to evaluate pixel-by-pixel correlation of signal intensity.Results and Discussion
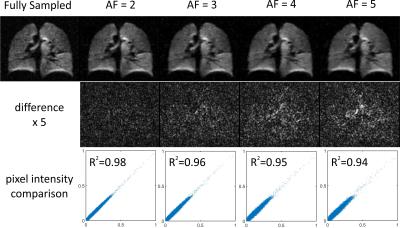
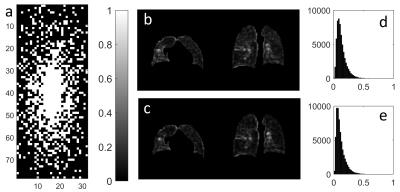
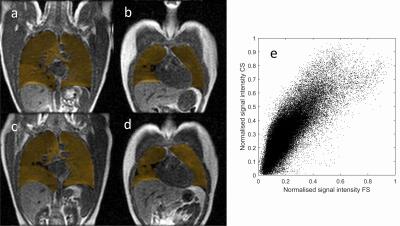
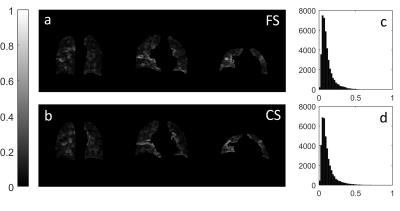
A good preservation of image details and quantitative ventilation metrics was observed in retrospectively undersampled datasets (Figure 1 and Table 1). As expected with higher AF, there was lesser agreement between FS and CS reconstructed data due to increase low-pass filtering of the images. This resulted in more homogeneous signal distributions and reduction of mean CoV (Figure 2 and Table 1). A CS sampling pattern with AF = 3 (Figure 2a) enabled a reduction of breath-hold time from 28 s to 15 s and was used for prospective acquisition of same breath HP 129Xe and 1H images. A difference of 0.4% in %VV (Figure 3) was found between prospective FS (95.8 %VV) and CS (96.2 %VV) dataset, which is well below the previously-calculated mean inter-observer error (7%) using the same software.10 Example slices of 129Xe CoV maps and histograms are shown in Figure 4. Mean (± standard deviation) CoV value of the ventilated lung were in good agreement (11.1 ± 8.3% for FS and 11.2 ± 8.9% for CS).Conclusion
We have demonstrated the feasibility of acquiring 3D HP 129Xe lung ventilation images and anatomical 1H images in the same breath using compressed sensing. A good qualitative agreement was found between a FS and prospective CS datasets and quantitative analysis of the images showed that %VV, pixel-by-pixel comparison of signal intensity and CoV histograms were in good agreement. This method is therefore ready for clinical evaluation in lung disease patients.Acknowledgements
No acknowledgement found.References
1. Horn F, et al. Lung ventilation volumetry with same-breath acquisition of hyperpolarized gas and proton MRI. NMR in biomedicine. 2014;27(12):1461-7.
2. Svenningsen S, et al. Hyperpolarized (3) He and (129) Xe MRI: differences in asthma before bronchodilation. J Magn Reson Imaging. 2013;38(6):1521-30.
3. He M, et al. Extending semiautomatic ventilation defect analysis for hyperpolarized (129)Xe ventilation MRI. Acad Radiol. 2014;21(12):1530-41.
4. Lustig M, et al. Sparse MRI: The application of compressed sensing for rapid MR imaging. Magn Reson Med. 2007;58(6):1182-95.
5. Ajraoui S, et al. Compressed sensing in hyperpolarized 3He lung MRI. 2010;63(4):1059-69.
6. Qing K, et al. Rapid acquisition of helium-3 and proton three-dimensional image sets of the human lung in a single breath-hold using compressed sensing. Magn Reson Med. 2015;74(4):1110-5.
7. Norquay G, et al. Approaching the theoretical limit for 129Xe hyperpolarisation with continuous-flow spin-exchange optical pumping. Proceedings of the 23rd Annual Meeting and Exhibition of the International society for magnetic resonance in medicine; 2015, 10-16 May; Toronto, ON, Canada, Program number 1505.
8. Stewart N, et al. Feasibility of human lung ventilation imaging using highly polarized naturally abundant xenon and optimized three-dimensional steady-state free precession. Magn Reson Med. 2015;74(2):346-352.
9. Tzeng Y, et al. The difference in ventilation heterogeneity between asthmatic and healthy subjects quantified using hyperpolarized 3He MRI. J Appl Physiol. 2009;106(3):813-22.
10. Hughes P, et al. Spatial Fuzzy C-Means Thresholding for Semi-Automated Calculation of Percentage Lung Ventilated Volume from Hyperpolarised Gas and 1H MRI. Proceedings of the 24th Annual Meeting and Exhibition of the International society for magnetic resonance in medicine; 2016 07-13 May; Singapore; Program number 1622.
Figures