2136
Utility of MRI for the Evaluation of Acute Pulmonary EmbolismAnthony Jedd1, James Costello1, Shannon Urbina1, Bobby Kalb1, and Diego Martin1
1Medical Imaging, Banner University Medical Center, Tucson, AZ, United States
Synopsis
CT-PA is the gold standard for diagnosis of pulmonary embolism, but requires use of radiation and iodinated contrast. There is an overall low incidence of positive studies (5%) in the patient population 18-45. Our study evaluates the negative predictive value of MRI as the primary imaging modality for exclusion of suspected PE in patients <40 y/o and/or relative contraindication to iodinated contrast. We found a negative predictive value of 99% in our patient population. These results suggest that MRI is an effective first-line imaging modality to exclude PE, while reducing exposure to ionizing radiation and iodinated contrast.
Purpose
To assess the negative predictive value (NPV) of magnetic resonance imaging (MRI) to exclude pulmonary embolism (PE) in patients presenting to the emergency department (ED) with suspected PE in the following categories: a) <40 years and/or b) contraindication to iodinated contrast.Methods
Retrospective study IRB-approved. A cross-departmental protocol was instituted to obtain MRI as the primary diagnostic modality for patients with clinical concern for PE that fit the following categories: a) ≤ 40 years old and/or b) contraindication to iodinated contrast. Patients were enrolled from January 2013 – December 2015. Exams performed on 1.5T system (Magnetom Aera). Chest imaging included 1) breath-hold (BH) contrast-enhanced 3D MR angiography, 2) BH 3D gradient echo (GRE) with 12° flip angle and 3) BH steady state free precession sequence, all in axial and coronal planes. Gadobenate dimeglumine administered at 0.1 mmol/kg mixed with an equal amount of saline and injected at 2 cc/s. Studies were interpreted by radiologist assigned to the clinical service and results were classified as a) positive, b) negative or c) indeterminate for PE. Patients with negative MRI were confirmed with a) phone interview at 3 months after MRI and b) review of medical records for subsequent PE or deep venous thrombosis (DVT). Patients with negative MRI were categorized as false negatives if the patient had documentation of PE or DVT within 3 months after MRI.Results
447 patients presented to ED with suspected PE and had MRI. 411/447 (92%) had negative MRI, and 36/447 (8%) had positive MRI for PE. Out of 411 patients with negative MRI, follow-up phone interview and records review at 3 months after presentation identified 3 patients developed subsequent PE or DVT. Subgroup analysis demonstrated 157/447 patients had eGFR < 45 at the time of imaging. Negative predictive value of MRI was 99% in our patient population.Discussion
Our study demonstrated safety and efficacy for using MRI to exclude pulmonary embolism in patients < 40 yo and also in patients with contraindication to iodinated contrast.Conclusion
MRI holds potential to improve patient safety by reducing exposure to ionizing radiation and iodinated contrast when imaging is required to exclude PE.Acknowledgements
No acknowledgement found.References
Schiebler ML, Nagle SK, Francois CJ, et al. Effectiveness of MR angiography for the primary diagnosis of acute pulmonary embolism: clinical outcomes at 3 months and 1 year. J Magn Reson Imaging 2013; 38(4):914-925.Figures

Axial 3D GRE post contrast MRI of the chest, which shows a
pulmonary embolism in the left lower pulmonary artery.
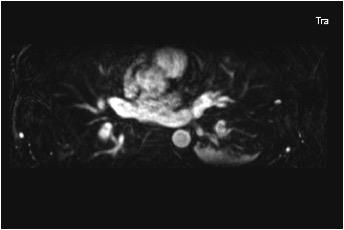
Axial 3D MRA MRI of the chest, which shows a pulmonary
embolism within the left lower pulmonary artery.
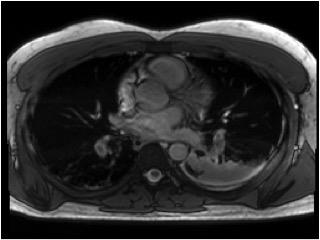
Axial SSFP MRI of the chest with pulmonary embolus
identified within the bilateral lower pulmonary arteries.