2124
Breast Background Parenchymal Enhancement as a Marker of Breast Cancer Recurrence Risk1Department of Radiology, Massachusetts General Hospital, Boston, MA, United States, 2Department of Medicine, Massachusetts General Hospital, Boston, MA, United States
Synopsis
Emerging studies suggest that imaging features could complement standard pathologic variables in cancer prognostic assessment. Studies on the association of background parenchymal enhancement (BPE) with breast cancer prognosis remain limited. The goal of this study was to investigate the complementary value of breast BPE as a prognostic marker for breast cancer recurrence risk assessment. DCE-MRI images were retrospectively analyzed from 100 women with breast cancer. Oncotype DX score was used as a surrogate for cancer recurrence. Our results suggest that BPE could complement histopathologic factors in predicting breast cancer recurrence risk and could potentially improve breast cancer prognostication.
Purpose
In the era of precision medicine, defining improved prognostic markers is essential to inform treatment decisions in patients afflicted with breast cancer. To date, pathologic evaluation and genetic profiling of tumor tissue remain the gold standard for providing information on the long-term clinical outcome of patients1-2. Recent studies have suggested that imaging features have the potential to capture information about underlying tumor biology that could complement standard pathologic assessment3-5. Particularly, background parenchymal enhancement (BPE) has recently emerged as a novel imaging biomarker associated with breast cancer risk6. Studies on the association of BPE with breast cancer prognosis remain limited. The goal of this study is to investigate the association between BPE and the risk of breast cancer recurrence as determined by Oncotype Dx7, a clinically-validated genomic test for assessment of 10-year breast cancer recurrence risk.Methods
We identified 100 women with a diagnosis of node-negative, ER/PR-positive, HER2-negative invasive breast cancer, who had breast MRI and concurrent Oncotype Dx results. Oncotype Dx generates a recurrence score based on the expression of 21 genes, stratifying patients into low, intermediate and high local recurrence risk categories. BPE was graded by an independent breast imager as minimal, mild, moderate or marked. Hormone therapy use, history of oophorectomy, menopausal status and patient’s age as well as tumor pathology data (tumor size, grade, multifocality, surgical margins and lymphatic invasion) were abstracted from chart review. The differences in BPE stratified by recurrence risk category were assessed using the Mann-Whitney test. Patients were grouped into an intermediate/high or a low recurrence risk category. A logistic regression model was used to assess the performance of BPE in predicting low and intermediate/high recurrence risk, with adjustment for potential hormonal confounders. To assess the role of BPE in contributing to recurrence risk category prediction, we compared the performance of a regression model that included standard pathologic and clinical prognostic variables to that of the same model incorporating BPE. Performance of the regression models was assessed using ROC curve analysis.Results and Discussion
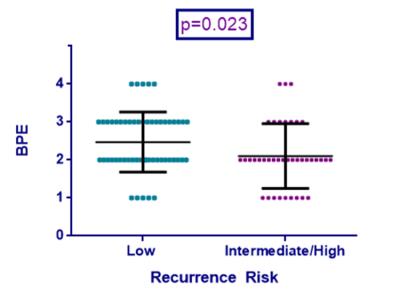
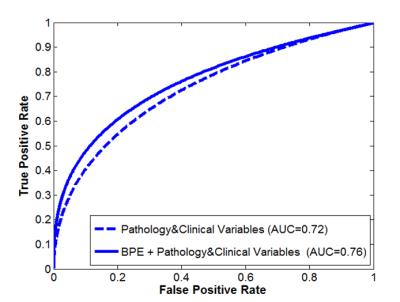
BPE is lower in patients with intermediate/high breast cancer recurrence risk (p=0.023). BPE significantly contributes to recurrence risk prediction (OR=0.57; p=0.037) and retains significant contribution after adjusting for potential hormonal confounders (OR=0.54; p=0.039). When combined with standard prognostic pathologic and clinical variables, BPE exhibits an independent contribution to recurrence risk prediction (OR=0.50; p=0.032) and improves the performance of the prediction model (AUC=0.76), when compared to a model that includes pathology and clinical variables only (AUC=0.72). Overall, our results suggest that the BPE can complement histopathologic factors in predicting breast cancer recurrence risk. Integrating BPE with standard histopathologic markers can potentially improve prognostic assessment for women diagnosed with breast cancer by adding information about the tumor microenvironment that may not be currently captured by standard prognostic markers.Conclusion
Low BPE is associated with increased breast cancer recurrence risk, as determined by Oncotype Dx. BPE independently contributes to recurrence risk prediction and complements standard clinical and pathologic variables. Breast background parenchymal enhancement has the potential to improve prognostic risk assessment and management of breast cancer patients.Acknowledgements
None
References
1. Paik et al., Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor–positive breast cancer, J Clin Oncol (2006).
2. Albain et al., Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial, Lancet Oncol (2010)
3. Loiselle et al., Dynamic contrast-enhanced magnetic resonance imaging and invasive breast cancer: Primary lesion kinetics correlated with axillary lymph node extracapsular extension, JMRI (2011)
4. Bathen et al., MR-determined metabolic phenotype of breast cancer in prediction of lymphatic spread, grade, and hormone status, Breast Can Res Treat (2007)
5. Szabo et al., Invasive breast cancer: correlation of dynamic MR features with prognostic factors, Eur Rad (2003)
6. King et al., Background parenchymal enhancement at breast MR imaging and breast cancer risk, Radiology (2011)
7. Paik et al., A multigene assay to predict recurrence of Tamoxifen-treated, node-negative breast cancer, NEJM (2004)
Figures