2121
Image quality of silicone-specific STIR Cube-FLEX MRI for breast implant imaging1Radiology, Stanford University School of Medicine, Stanford, CA, United States, 2Radiology, Rakuwakai Otowa Hospital, Kyoto, Japan, 3GE Medical Systems
Synopsis
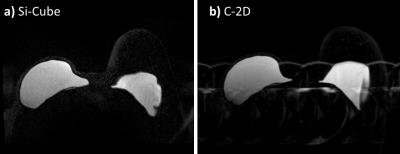
3D Fast-Spin-Echo MRI with Short Tau inversion recovery fat suppression and 2-point Dixon decomposition of water and silicone signal (STIR Cube-FLEX or “Si-Cube”) is a recently developed silicone-specific sequence providing isotropic, high-resolution 3D datasets that are easily reformatted into any plane. We performed a reader study to evaluate the image quality of Si-Cube in 39 females, and found Si-Cube is robust to artifacts and has equivalent image quality to conventional 2D silicone-specific sequences (C-2D). The ability to reformat Si-Cube images in any plane potentially obviates the need to obtain C-2D sequences in other planes, streamlining the overall implant imaging protocol.
Introduction
Three-dimensional Fast-Spin-Echo MRI with Short Tau inversion recovery (STIR) fat suppression and 2-point Dixon decomposition of water and silicone signal (STIR Cube-FLEX or “Si-Cube”) (Figure 1) is a recently developed 3D silicone-specific imaging method providing isotropic, high-resolution 3D datasets that are easily reformatted into any plane, with a shorter acquisition time than silicone-specific STIR Cube IDEAL1, and that are robust to B0 field inhomogeneity. The aim of this study was to evaluate the image quality of Si-Cube compared to conventional 2D silicone-specific STIR (C-2D) sequences based on visual assessment.
Methods
From 149 Si-Cube studies performed between March 2014 and February 2016, we retrospectively selected consecutive patients undergoing both Si-Cube and C-2D MR imaging (water-saturated STIR fast spin-echo2, or STIR fast spin-echo with iterative decomposition of silicone and water using least-squares approximation [STIR-IDEAL3,4]). Axial planes were used for the visual assessment, and Si-Cube and C-2D images were placed side by side for comparison. Three experienced breast radiologists independently evaluated images for quality of fat suppression, uniformity of fat suppression, quality of water suppression, brightness of silicone signal, uniformity of silicone signal, clarity of chest wall envelope surface, visualization quality of radial folds, perceived signal to noise ratio, artifacts (ghost artifacts of breasts and the heart, wraparound artifacts, SWAP artifacts, B1+ inhomogeneity, overall artifacts), and overall image quality using 5-point scales. Wilcoxon signed-rank test was performed to compare the scores between Si-Cube and C-2D in each reader, and when the same significant tendency was constantly observed in at least two readers, the difference between Si-Cube and C-2D was finally considered as significant.Results
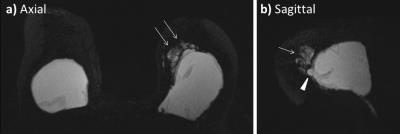
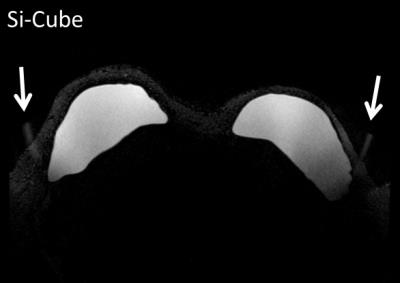
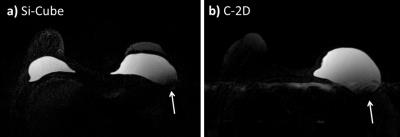
A total of thirty-nine patients were identified. C-2D sequences included water-saturated STIR fast spin-echo (n=23) and STIR-IDEAL (n=16). There were no significant differences in any image quality categories except for artifacts. Ghost artifacts of breasts and the heart were more common and severe in C-2D than in Si-Cube (p<0.01 in all three readers) (Figure 2). Moderate to severe ghost artifacts of breasts and those from heart were observed in 0-33% and 59-95% of cases, respectively, in C-2D, while never in Si-Cube. Wraparound artifacts were not frequent in both images, with the frequency of severe to moderate wraparound artifacts of 0-10% in Si-Cube and 0-8% in C-2D, but were slightly more common in Si-Cube than C-2D (p<0.05 in two) (Figure 3). SWAP artifacts were rare in both. Moderate to severe B1+ inhomogeneity was observed in 13-36% in Si-Cube and in 10-21% in C-2D without a significant difference (Figure 4). Overall artifacts were significantly more prominent in C-2D than Si-Cube (p<0.01 in three). Overall image quality was acceptable to excellent in 74-90% for Si-Cube and 64-77% for C-2D, and no significant difference was identified between Si-Cube and C-2D.Discussion
Our data demonstrated that the image quality of Si-Cube was at least equivalent to C-2D. We did note Si-Cube was robust to ghost artifacts, which were common in C-2D. This is probably because Si-Cube is a volumetric 3D acquisition; respiratory and cardiac motion are averaged over the entire acquisition time rather than over the limited number of shots required for each slice in 2D imaging. As previously reported, expected advantages of the Dixon techniques include that they can compensate for effects of field inhomogeneities during the image reconstruction process and thus are insensitive to B0 field inhomogeneity3. However, in our series, B1+ inhomogeneity was observed in Si-Cube as often as in C-2D. This reflects the retrospective nature of our study. Additional analysis showed moderate to severe B1+ inhomogeneity on Si-Cube mostly occurred in the first 16 months after the implementation of Si-Cube, before transmit hardware was upgraded to improve B1+ uniformity, and was rare afterwards.Conclusion
Si-Cube may be a useful silicone-specific MRI sequence with acceptable image quality and less artifacts than C-2D. The ability to reformat Si-Cube images in any plane potentially obviates the need to obtain C-2D sequences in other planes, streamlining the overall implant imaging protocol.Acknowledgements
No acknowledgement found.References
1. Madhuranthakam AJ, Smith MP, Yu H, et al. Water-silicone separated volumetric MR acquisition for rapid assessment of breast implants. J Magn Reson Imaging. 2012;35(5):1216-21.
2. Mukundan S Jr, Dixon WT, Kruse BD, Monticciolo DL, Nelson RC. MR imaging of silicone gel-filled breast implants in vivo with a method that visualizes silicone selectively. J Magn Reson Imaging. 1993;3(5):713-7.
3. Ma J, Choi H, Stafford RJ, Miller MJ. Silicone-specific imaging using an inversion-recovery-prepared fast three-point Dixon technique. J Magn Reson Imaging. 2004;19(3):298-302.
4. Kim SH, Lipson JA, Moran CJ, et al. Image quality and diagnostic performance of silicone-specific breast MRI. Magn Reson Imaging. 2013;31(9):1472-8.
Figures