2092
3D T2-weighted fast spin echo (FSE) with outer volume suppression versus 2D FSE in the prostate: Comparison of lesion detection in the transition zone and image quality1Radiology, Stanford University, Stanford, CA, United States, 2Global MR Applications and Workflow, GE Healthcare, 3Electrical Engineering and Radiology, Stanford University, Stanford, CA, United States
Synopsis
3D T2-weighted imaging (T2WI) of the prostate for prostate cancer (PCa) is often hampered by motion artifacts and signal starvation. However, incorporating reduced phase field of view capability using outer volume suppression (OVS) into 3D fast spin echo (FSE) can overcome these obstacles. In the prostatic transition zone (TZ), superior contrast and diminished blur were found over standard 2D FSE, with preserved SNR and anatomic detail. Diagnostic confidence was greater with 3D, whether used alone or in combination with 2D. Furthermore, less equivocal diagnoses resulted with the combination of 2D and 3D.
Introduction
Approximately 30% of prostate cancer (PCa) occurs in the transition zone (TZ), which may be undersampled in transrectal ultrasound-guided (TRUS) biopsies. Accuracy of biopsy improves when TRUS technique is combined with multiparametric magnetic resonance imaging (mpMRI) of the prostate, allowing targeted biopsy of mpMRI-identified lesions.1
The TZ comprises the majority of gland volume in older men, due to benign prostatic hyperplasia (BPH). BPH results in the characteristic “organized chaos” appearance of the TZ, making evaluation extremely challenging. Due to BPH, diffusion-weighted and postcontrast T1-weighted imaging is of limited utility, and acquiring high-quality T2WI is of paramount importance. Prostate Imaging Reporting and Data System (PI-RADS) was developed as an aid to mpMRI interpretation.2 PI-RADS lesion scoring is zonal dependent, with TZ evaluation almost completely dependent on T2WI, reflective of the difficulty arising from BPH.
Standard T2WI is a 2D axial fast spin echo (FSE) acquisition. Despite the primacy of T2WI in the TZ, superiority of 2D versus 3D FSE remains unknown. Previous efforts at 3D FSE have been hampered by motion artifacts and signal starvation and have focused on the peripheral zone (PZ) where T2WI has a near nonexistent role.3,4 A recently developed 3D FSE acquisition employs outer volume suppression (OVS), allowing excitation and spatial encoding only around the prostate, overcoming motion and scan time limitations.5 We hypothesized that TZ image quality, anatomic delineation and lesion detection would be superior on 3D in comparison to 2D FSE.
Methods
This was an IRB-approved, HIPAA-compliant retrospective study of patients who underwent 3D FSE with OVS and standard 2D FSE during mpMRI. Fat saturation was applied in 3D T2WI for better prostate visualization. Exclusion criteria included prior prostatectomy and brachytherapy.
Three radiologists independently assessed individual T2WI series for image quality (1-4; inferior-superior) and anatomic delineation (1-5; inferior-superior). TZ lesion detection conformed to PI-RADS v2 with diffusion-weighted imaging (DWI) and apparent diffusion coefficient (ADC) maps available. Diagnostic confidence was also scored (1-5; low-high). Subsequently, lesions identified on 2D were reevaluated with simultaneous 2D + 3D viewing.
Inter-reader agreement was evaluated with intraclass correlation coefficients (ICC). Wilcoxon signed rank tests were performed for paired, nonparametric analyses of ordinal variables with a Bonferroni-Holm correction for multiple comparisons. McNemar’s test assessed for differences in frequency of lesion detection.
Results
The final cohort consisted of 19 patients: average age of 66.9 ± 7.0 years and prostate-specific antigen (PSA) of 9.09 ± 4.77 ng/mL. Clinical indications included staging of known high-risk PCa (7/19), active surveillance of low-risk PCa (5/19), elevated PSA (5/19), abnormal digital rectal exam (1/19), or unspecified (1/19).
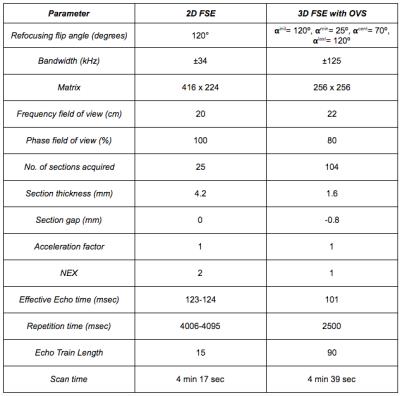
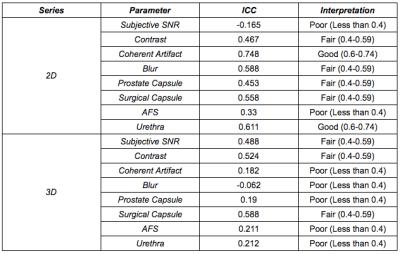
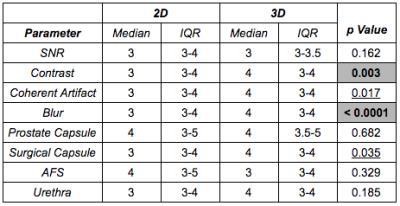
Inter-reader agreement of image quality and anatomic parameters was greater for 2D than 3D, possibly due to reader unfamiliarity with the 3D series (Table 1). However, in comparison with 2D, superior contrast and reduced blur were noted on 3D; no significant difference in SNR was detected (Table 2).
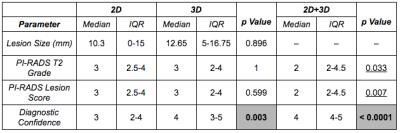
74% (42/57) of interpretations were consistent across both series (Table 3). 2D revealed 37 lesions and 3D only 28; all 24 lesions identified on both series represented the same lesion. Both frequency of detection and total number of lesions detected were greater on 2D (p = 0.022 and p = 0.039, respectively).
Lesion assessment did not differ by series (Table 4). Nonetheless, PI-RADS lesion scores trended towards being significantly lower on 2D + 3D versus 2D alone (Figure 1). Furthermore, incidence of PI-RADS lesion score 3 – indicating equivocality for PCa and diagnostic ambiguity – dropped nearly 85% with 2D + 3D versus 2D alone (p = 0.003). Diagnostic confidence was greater on 2D + 3D over 2D alone and on 3D than 2D.
Discussion
We found that 3D FSE incorporating OVS improves contrast and decreases blur over 2D FSE while preserving SNR and anatomic detail of the TZ. This improves upon previous attempts, appropriately implementing the technique in TZ lesion evaluation in keeping with PI-RADS methodology. 3D FSE is not only viable as far as scan time and image quality but also increases diagnostic confidence and decreases diagnostic ambiguity when used in combination with 2D FSE.
As our cohort undergoes MR/Ultrasound fusion biopsy, clinical significance of less lesion detection by 3D, apparent trend towards lesion down-scoring on 2D + 3D, and decreased equivocal scoring will become known. We hypothesize these result from better detection of benign characteristics on 3D FSE.
Conclusion
3D FSE incorporating OVS is clinically feasible with superior contrast and less artifacts in the TZ than 2D FSE while preserving SNR. Beyond multiplanar reconstructions afforded by 3D imaging, 3D increases diagnostic confidence and may better identify benign lesion characteristics.Acknowledgements
The authors would also like to thank the support of GE Healthcare.References
1. Le JD, Stephenson S, Brugger M, et al. Magnetic resonance imaging-ultrasound fusion biopsy for prediction of final prostate pathology. J Urol. 2014;192:1367-1373.
2. Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging-Reporting and Data System: 2015, Version 2. Eur Urol. 2016;69:16-40.
3. Gupta RT, Spilseth B, Patel N, Brown AF, Yu J. Multiparametric prostate MRI: focus on T2-weighted imaging and role in staging of prostate cancer. Abdom Radiol. 2016;41:831-843.
4. Rosenkrantz AB, Neil J, Kong X, Melamed J, Babb JS, Taneja SS, Taouli B. Prostate cancer: comparison of 3D T2-weighted with conventional 2D T2-weighted imaging for image quality and tumor detection. AJR Am J Roentgenol. 2010;194;446-452.
5. Han M, Chiba K, Banerjee S, Carballido-Gamio J, Krug R. Spin-echo sequence combined with outer volume suppression for imaging trabecular bone structure of the proximal femur. J Magn Reson Imaging. 2015;41:1300-1310.
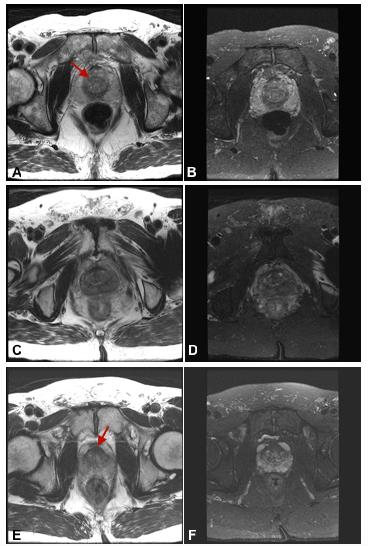
Figures