2091
Evaluation of Prostate Imaging Reporting and Data System version 2 (PI-RADS v2) in predicting clinically significant prostate cancer: a whole-mount step-section analysisWang Huihui1 and Wang Xiaoying1
1Peking University First Hospital, Beijing, People's Republic of China
Synopsis
The diagnostic accuracy of PI-RADS v2 for clinically significant cancer was evaluated by using whole-mount step-section slides as standard of reference. All significant cancers could be identified and the accuracy of PI-RADS 3 to 5 for predicting significant cancer was 91.7%, with high sensitivity (100%) and negative predictive value (100%).
Introduction
Prostate Imaging Reporting and Data System version 2 (PI-RADS v2) is designed to promote global standardization in the interpretation of prostate mpMRI examinations. But the dignostic feasibility and performance need to be evaluated by further data and experience. To evaluate the diagnostic accuracy of PI-RADS v2 for clinically significant cancer on multiparametric MRI (mpMRI) by using whole-mount step-section slides as standard of reference.Materials and methods
Thirty-six consecutive patients with biopsy-proven prostate cancer (PCa) were included. All patients received prostatic mpMRI (GE 3.0 T Signa TwinSpeed, 3.0 T Discovery HD 750 and PHILIP Achieva 3.0 T TX), including T2WI, DWI and DCE. All patients received no endocrine therapy, chemotherapy, radiation therapy or any other kinds of therapy. Following radical prostatectomy, all specimens were processed as whole-mount step-section slides. MR images were interpreted according to PI-RADS v2 by an experienced radiologist who was blinded to clinical details and histopathology. Index lesion was analyzed and correlated with histopathologic findings by using side-by-side comparison. In mpMRI, the definition of index lesion was the lesion with highest PI-RADS score in the gland. In pathology slides, the definition of clinically significant cancer was defined as tumor with Gleason score≥7, volume≥0.5 cc and/or extraprostatic extension (EPE).Results
The mean age was 65.1±7.3 years. The range of PSA was 5.70-50.52 ng/ml. There were 32 clinically significant cancers and 4 clinically insignificant cancers in 36 index lesions. And 27.8% of patients PCa with biopsy-proven were upgraded postoperatively (Table 1). Only one lesion was scored PI-RADS 2 and the histopathology was clinically insignificant cancer (Gleason score=3+2). The accuracy of PI-RADS 3 to 5 for predicting significant cancer was 91.7%. The negative predictive value (NPV) and positive predictive value (PPV) were 100% and 91.4%, with a sensitivity of 100% and specificity of 25.0% (Table 2). Overall PI-RADS scoring system showed moderate diagnostic accuracy for significant cancer detection (area under the curve 0.875, P=0.016, 95% confidence interval 0.727-1.000, Figure 2).Discussion and Conclusion
In this study, we have found that the high sensitivity and NPV of PI-RADS v2 imply a potential role for mpMRI in detecting clinically significant prostate cancer (Figure 1). All clinically significant prostate cancers were identified according to PI-PADS v2 when PI-RADS Assessment Category ≥3 were considered to be positive. Gleason score is the most important factor for predicting prognisis of prostate cancer. Biopsy provides a sufficiently high specificity for diagnosis but limited sensitivity. In our study, 13.9% of GS 6 were upgraded to GS≥7 and the total rate of GS upgrading was 27.8%. MpMRI provides more extensive evaluation of prostate gland than biopsy, and PI-RADS v2 improves the diagnostic accuracy of clinically significant cancer.Acknowledgements
No acknowledgement found.References
1. Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging-Reporting and Data System: 2015, Version 2. Eur Urol. 2016,69(1):16-40. 2. Kasel-Seibert M, Lehmann T, Aschenbach R, et al. Assessment of PI-RADS v2 for the Detection of Prostate Cancer. Eur J Radiol. 2016,85(4):726-31.Figures
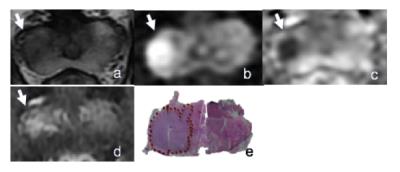
Figure 1. A 74 years old man with clincally
significant prostate cancer. Serum PSA level was 11.79 ng/ml. (a–d) T2-weighted
imaging, diffusion weighted imaging (DWI), apparent diffusion coefficient (ADC)
map and dynamic contrastenhanced (DCE) imaging showed a focal lesion in the
right peripheral zone of the prostate gland (arrow). (e) The lesion was
analyzed on the whole-mount step section pathology and GS was 4+3, with
tertiary 5 (red dotted circle). PI-RADS Assessment Category was 4 by the Reader.
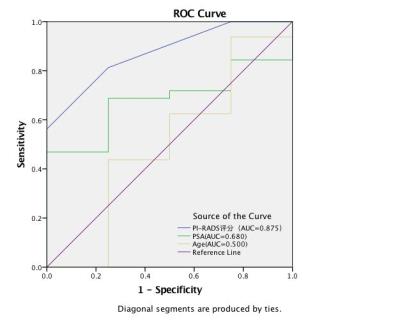
Figure
2. AUCs of PSA, age and PI-RADS to predict significant PCa at prostatectomy specimens.
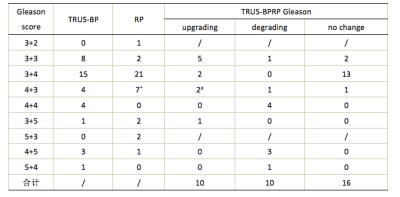
Table 1. Comparasion of biopsy and prostatectomy Gleason score.
* Tertiary GS 5 found in 4 cases. # Tertiary GS 5 found in 1 case.
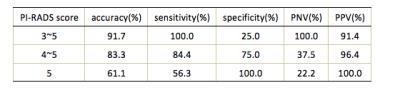
Table 2. Accuracy,
Sensitivity, Specificity, NPV and PPV of PI-RADS 3-5 detection of clinically
significant PCa