2083
Association of breastfeeding duration with abdominal fat distribution and adipose tissue hydration at 4.5 years1Singapore Institute for Clinical Sciences, A*STAR, Singapore, 2Department of Obstetrics & Gynaecology, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 3Singapore BioImaging Consortium, A*STAR, Singapore, 4Department of Paediatrics, Yong Loo Lin School of Medicine, National University of Singapore, Singapore, 5Department of Paediatric Endocrinology, KK Women’s and Children’s Hospital, Singapore, 6Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, 7MRC Lifecourse Epidemiology Unit & NIHR Southampton Biomedical Research Centre, University of Southampton & University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom, 8Clinical Nutrition Research Centre, Singapore Institute for Clinical Sciences, A*STAR, Singapore, 9Department of Endocrinology, Tan Tock Seng Hospital, Singapore, 10Liggins Institute, University of Auckland, Auckland, New Zealand, 11Department of Diagnostic and Interventional Imaging, KK Women’s and Children’s Hospital, Singapore
Synopsis
The association of the duration of breastfeeding with childhood obesity is equivocal. The first year of life is a period of hypertrophic expansion of adipocytes with little increase in adipocyte number. Hence, over-nutrition during this period could potentially result in persistent changes in adipocyte size that may last until adulthood. In this study, we have investigated the association of breastfeeding duration with abdominal fat distribution and adipose tissue cellularity at 4.5 years. Our results indicate a weak protective effect of longer breastfeeding duration on abdominal subcutaneous adipose tissue volumes and subcutaneous adipose tissue morphology.
Introduction
The association of the duration of breastfeeding with childhood obesity is equivocal [1-3]. Most of the prior studies on the effect of breastfeeding on childhood adiposity have relied on anthropometric indices like BMI-for-age, with very few studies actually measuring the adipose depot volumes [4]. The effect of breastfeeding duration on adipose tissue morphology has also not been well investigated. A hypertrophic adipose tissue profile, with large adipocytes has been linked to poor metabolic health [5]. The first year of life is a period of hypertrophic expansion of adipocytes with little increase in adipocyte number [6]. Hence, over-nutrition during this period could potentially result in persistent changes in adipocyte size that may last until adulthood. We have previously shown that the adipose tissue hydration, assessed by 1H MRS, is related to its morphological status, with low hydration levels reflecting increased adipocyte hypertrophy [7]. In this study, we have investigated the association of breastfeeding duration with abdominal fat distribution and adipose tissue hydration at 4.5 years.Methods
We studied 316 subjects (158 Chinese, 94 Malay and 64 Indian; 150 boys and 166 girls) aged 4.5 years participating in the Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort [8]. The infant feeding patterns during the first year were recorded as exclusive breastfeeding, partial breastfeeding or exclusive formula feeding from the mothers. The data were recoded as a binary variable indicating the duration of any (exclusive or partial) breastfeeding (< 3 months and ≥ 3 months). The subjects underwent MRI of the abdomen without sedation on the Siemens Skyra 3T MR scanner with Syngo VE 11A software. Sixty axial slices with 5-mm slice thickness and in-plane resolution of 0.94 × 0.94 mm were acquired using water-suppressed HASTE sequence (TR=1000 ms, TE=95 ms) and body matrix coil. A fully-automated graph theoretic segmentation algorithm [9] was used to segment and quantify the SAT and IAT depots between the liver dome and upper sacrum. The output image was then edited manually to remove bowel and other misclassified structures. The deep (DSAT) and superficial (SSAT) subcutaneous adipose tissue depots were segmented manually. The volume-localized 1H MR spectrum of DSAT was obtained from a 1 × 1 × 1 cm3 voxel at the level of the L5 lumbar vertebra using PRESS sequence (TR=2000 ms, TE=30 ms, 8 avg). The resonances were fitted and quantified using an in-house Matlab program. The adipose tissue hydration was assessed using hydrolipidic ratio (HLR) defined as (water/(water+fat)).
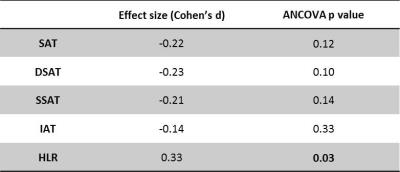
We evaluated the effect of
duration of breastfeeding on abdominal fat volumes (SAT, SSAT, DSAT and IAT)
and adipose tissue HLR, after adjusting for ethnicity, gender, maternal age,
maternal prepregnancy BMI, birth weight-for-gestational-age status and maternal
education. The Cohen’s d effect size measure [10] of breastfeeding duration was
evaluated as the difference in the adjusted means, standardized by the square
root of the mean square error of the ANCOVA model. The following thresholds
were used to assess the practical significance of the effect size, large effect:
Cohen’s d ≥ 0.8, moderate effect: Cohen’s d ≥ 0.5, small effect: Cohen’s d ≥ 0.2.
Results and Discussion
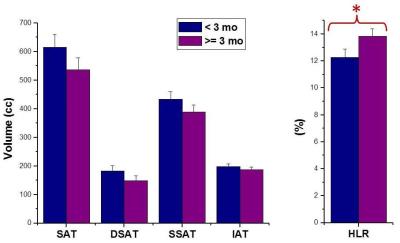
The adjusted means of the adipose depot volumes and HLR are shownin Figure 1. We found a small negative effect of longer breastfeeding duration (≥ 3 months) on total SAT, DSAT and SSAT volumes and a small positive effect on HLR (Table 1). The effect of breastfeeding duration on IAT was not practically significant.
The expansion of adipose tissue during the first year of life is predominantly through increment in adipocyte size than number. Studies have shown that in children who get obese at this stage, this increased adipocyte size remains unchanged until early adulthood [6]. This altered adipose tissue cellularity in childhood could have an effect on impaired metabolic health in adult life. Hence, over-nutrition during the first year of life could create persistent changes in adipose tissue morphology. Our results indicate a weak protective effect of longer breastfeeding duration on abdominal SAT volumes and subcutaneous adipose tissue morphology. These results are in line with studies indicating a small protective effect of breastfeeding on childhood obesity [11]. We note that our study does not allow us to rule out ‘reverse causality’ [12]. Infants who were accumulating more abdominal fat and had increased adipocyte hypertrophy could potentially influence feeding decisions using behavioral cues (crying, showing signs of hunger) and prompt early supplementation/weaning.
Acknowledgements
This research is supported by the Singapore National Research Foundation under its Translational and Clinical Research (TCR) Flagship Programme and administered by the Singapore Ministry of Health’s National Medical Research Council (NMRC), Singapore- NMRC/TCR/004-NUS/2008; NMRC/TCR/012-NUHS/2014. Additional funding is provided by the Singapore Institute for Clinical Sciences, Agency for Science Technology and Research (A*STAR), Singapore.References
1. Yan J, Liu L, Zhu Y, Huang G, Wang PP. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health 2014, 14(1):1.
2. Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG. The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. The American journal of clinical nutrition 2005, 82(6):1298-307.
3. Kramer MS, Matush L, Vanilovich I, Platt RW, Bogdanovich N, Sevkovskaya Z, Dzikovich I, Shishko G, Collet JP, Martin RM, Smith GD. A randomized breast-feeding promotion intervention did not reduce child obesity in Belarus. The Journal of nutrition 2009, 139(2):417S-21S.
4. Crume TL, Bahr TM, Mayer-Davis EJ, Hamman RF, Scherzinger AL, Stamm E, Dabelea D. Selective protection against extremes in childhood body size, abdominal fat deposition, and fat patterning in breastfed children. Archives of pediatrics & adolescent medicine 2012, 166(5):437-43.
5. Henninger AJ, Eliasson B, Jenndahl LE, Hammarstedt A. Adipocyte hypertrophy, inflammation and fibrosis characterize subcutaneous adipose tissue of healthy, non-obese subjects predisposed to type 2 diabetes. PloS one 2014, 9(8):e105262.
6. Knittle JL, Timmers K, Ginsberg-Fellner F, Brown RE, Katz DP. The growth of adipose tissue in children and adolescents. Cross-sectional and longitudinal studies of adipose cell number and size. Journal of Clinical Investigation 1979, 63(2):239.
7. Navin M et al. Adipose tissue hydration as a potential non-invasive marker for adipose tissue hypertrophy. Annual Meeting of the International Society for Magnetic Resonance in Medicine (ISMRM) 2015, p.0840.
8. Soh SE et al. Cohort profile: Growing Up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. International journal of epidemiology 2014, 43:1401-1409.
9. Sadananthan SA et al. Automated segmentation of visceral and subcutaneous (deep and superficial) adipose tissues in normal and overweight men. Journal of magnetic resonance imaging 2015, 41(4):924-34.
10. Cohen J. Statistical power analysis for the behavioral sciences (revised ed.) 1977.
11. Dewey KG. Is breastfeeding protective against child obesity? Journal of Human Lactation 2003, 19(1):9-18.
12. Kramer
MS, Moodie EE, Dahhou M, Platt RW. Breastfeeding and infant size: evidence of
reverse causality. American Journal of Epidemiology 2011, 173(9):978-83.