2064
Diagnostic accuracy of 3-T magnetic resonance imaging with Star VIBE: versus computer tomography in pulmonary nodules1The first affiliated hosptial of Shaanxi traditional chinese medical university, Xian Yang, People's Republic of China
Synopsis
Star VIBE (MRI) sequence in obtaining scan under free breathing can provide high-resolution imaging. Therefore, we assessed the accuracy of magnetic resonance imaging (MRI) for detecting pulmonary nodules by comparing the detection rate of high-resolution Star vibe sequence with the MSCT results. We concluded that pulmonary nodules with the maximum diameter more than 3mm can be detected by star-vibe (MRI) sequence with a satisfactory accuracy. Although pulmonary nodules with the max diameter less than 3mm had relatively low sensitivity, the accurate treatment decisions may also be made.
PURPOSE:
Multi slice spiral CT (MSCT) play a crucial role in detect pulmonary nodule with high sensitivity. However CT examination may produce high cumulative radiation doses by repetitive imaging for those patients with pulmonary nodule who need longitudinal observation. Given the improved soft tissue contrast and the lack of ionizing radiation, magnetic resonance imaging (MRI) is also suggested to be a means of diagnostic tool for pulmonary nodules [1,2]. Additionally, Star VIBE (MRI) sequence in obtaining scan under free breathing can provide high-resolution imaging. Therefore, we assessed the accuracy of magnetic resonance imaging (MRI) for detecting pulmonary nodules by comparing the detection rate of high-resolution Star vibe sequence with the MSCT results.
METHODS
The records of 12 patients with multiple pulmonary nodules detected by MSCT were enrolled in our study. Subjects were eligible to participate in the study if they were older than18 years, the presence of pulmonary nodule confirmed by MSCT scan, ability to undergo MRI and participate in the study. Exclusion criteria were contraindications to MR imaging such as pacemakers, metal implants. Star vibe MRI imaging was acquired less than 48h after HRCT. The MRI protocol (MAGNETOM 3.0T SKYRA MR scanner, Siemens healthcare, Erlangen, Germany) included a T2-weighted-tirm HASTE sequence (TE/TR:106 ms/∞, slice thickness 5mm) and a Prototyped T1-weighted 3D Star VIBE sequence(TE/TR:1.39/2.79,slice thickness 1.2mm).A total of 698 nodules were analyzed by one radiologist on MSCT (presence, maximum diameter, location and mean density) as the reference standard, and compared to the findings of MRI observed by a second radiologist, who was blinded to the MSCT results.RESULTS:
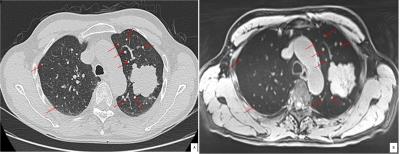
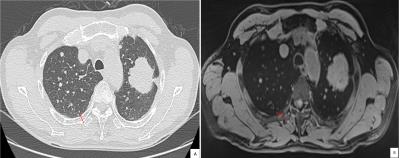
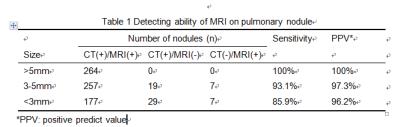
Pulmonary nodules were classified by the maximum diameter of nodules based on MSCT, which showing the total of 264 nodules with the maximum diameter more than 5mm; 276 nodules with the diameter between 3mm to 5mm; and 206 nodules with the diameter less than 3mm. Pulmonary nodules detected by MRI with the maximum diameter more than 5mm had the sensitivity of 100% and positive predict value of 100%;pulmonary nodules with the maximum diameter between 3mm to 5mm had the sensitivity of 93.1% and positive predict value of 97.3% (figure1); and nodules less than 3mm had the sensitivity of 85.9% and positive predict value of 96.2% (figure2, table1). MRI had limitations in detecting fully calcified nodule, and nodules located near heart and diaphragmatic surface, however, some sub-pleural nodules and small lymph nodes showed in MRI were not visualized by MSCT.CONCLUSION
Pulmonary nodules with the maximum diameter more than 3mm can be detected by star-vibe (MRI) sequence with a satisfactory accuracy. Although pulmonary nodules with the max diameter less than 3mm had relatively low sensitivity, the accurate treatment decisions may also be made.Acknowledgements
We would like to show our thanks to Dr Wang Shaoyu, who has provided us with valuable guidance in this work.References
[1] Schaarschmidt B, Buchbender C, Gomez B, Rubbert C, Hild F, Köhler J, et al. Thoracic staging of non-small-cell lung cancer using integrated (18)F-FDG PET/MR imaging: diagnostic value of different MR sequences. Eur J Nucl Med Mol Imaging. 2015; 42(8):1257-67.
[2] Chandarana H1, Block KT, Winfeld MJ, Lala SV, Mazori D, Giuffrida E, Babb JS, Milla SS. Free-breathing contrast-enhanced T1-weighted gradient-echo imaging with radial k-space sampling for paediatric abdominopelvic MRI. Eur Radiol. 2014; 24(2):320-6
Figures