2026
Evaluation of gravity effect on portal venous flow using multi-posture MRI1Radiology, Kanazawa University Graduate School of Medicine, Kanazawa, Japan, 2Division of Health Sciences, Kanazawa University Graduate School of Medical Sciences, Kanazawa, Japan
Synopsis
Portal venous flow (PVF) seems to be affected by gravity, ie., it depends on the body posture. We validated the effect of gravity on PVF in supine and upright positions using an original multi-posture MRI. We compared maximum PVF, PVF velocity, PVF volume, and cross-sectional area of portal vein between supine and upright positions. The mean PVF velocity, PVF volume, maximum PVF, and cross-sectional area in the upright position were significantly lower than those in the supine position. Gravity reduces PVF velocity and volume, and these differences between postures potentially provide new diagnostic information.
Purpose
Portal venous flow (PVF) is clinically important in liver function.1, 2 PVF may be affected by gravity, ie., it depends on body posture, but this has yet to be confirmed. In this study, we evaluated the effect of gravity on PVF in people in the supine and upright positions using an original magnetic resonance imaging (MRI) system that can obtain images in any posture (multi-posture MRI).Materials and Methods
Caval velocity-mapped images in eight healthy volunteers were obtained with ECG-triggered cine phase-contrast technique in the supine and upright positions using multi-posture MRI (Fig. 1). The mean PVF velocity in the region of interest in each cardiac phase was determined after correction by subtraction of the baseline offset due to eddy currents. In addition, a PVF curve in the cardiac cycle was obtained from the PVF-velocity multiplied by the cross-sectional area, and the PVF volume was calculated by integration of the PVF curve in the cardiac cycle. The maximum PVF (PVFmax), PVF velocity, PVF volume, and cross-sectional area of the portal vein in the supine and upright positions were assessed.Results and Discussion
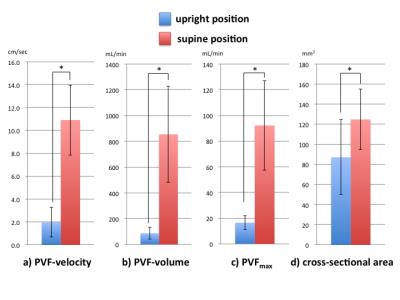
The mean PVF velocity in the upright position (1.96 ± 1.29 cm/sec) was significantly lower than that in the supine position (10.1 ± 3.06 cm/sec) (P < .05) (Fig. 2a). The mean PVF volume in the upright position (87.2 ± 46.2 mL/min) was significantly lower than that in the supine position (854 ± 374 mL/min) (P < .05) (Fig. 2b). The PVFmax in the upright position (16.5 ± 5.30 mL/min) was significantly lower than that in the supine position (92.2 ± 34.9 mL/min) (P < .05) (Fig. 2c). These results indicate that gravity reduced the PVF velocity and volume, and these differences between postures potentially provide new diagnostic information on the compensatory faculty of gravity as compared with standard PVF measurements. In addition, the mean cross-sectional area in the upright position (90.1 ± 37.4 mm2) was significantly lower than that in the supine position (125 ± 30.1 mm2) (P < .05) because of the regulation of the portal pressure (Fig. 2d).Conclusion
Gravity reduces PVF velocity and volume. Multi-posture MRI makes it possible to evaluate the effect of gravity on PVF.Acknowledgements
No acknowledgement found.References
1. Brauer, R.W. Liver circulation and function. 111, 57. Physiol. Rev. 1962: 43: 115-213
2. Itai Y, Matsui 0 :Blood flow and liver imaging. Radiology 1997: 202: 306-314
Figures